Translate this page into:
Prevalence of Fluorosis and pattern of Domestic filters use in two Fluoride endemic blocks of West Bengal, India
Address for correspondence: The Editor/ Managing Editor, Journal of Comprehensive Health Dept of Community medicine NRS Medical College, 138, AJC Bose Road, Kolkata-700014
Corresponding author: Dr. Kunal Kanti Majumdar, Dept. of Community Medicine, KPC Medical College & Hospital, Jadavpur, Kolkata E Mail- kunalmajumdar1@gmail.com kunalkm2003@yahoo.com
Abstract
Fluorosis is an impending public health problem in West Bengal affecting a large number of population, and Birbhum is one of the affected districts with seven affected blocks with increased prevalence of dental, skeletal, and non-skeletal fluorosis.
Objective:
The present study was conducted to see the extent of fluorosis in two selected affected blocks of Birbhum District of West Bengal and to determine the pattern of usage of domestic filters by the villagers of the above selected endemic villages.
Methodology:
A total 30 families were selected randomly out of families having past history of taking water from an unsafe source from the two endemic blocks i.e. Rampurhat I and Khoerasol of Birbhum Distric of West Bengal. Out of these 30 families a total 125 family members were selected health survey. A total 60 school children were examined and screened for Dental fluorosis in the above blocks. All these families were supplied domestic filters for removal of fluoride and the pattern of usage of domestic filters by the villagers were also studied.
Results:
44.4% and 47.5% of the study population are found to be suffering from Dental fluorosis. Prevalence of manifestations of skeletal fluorosis was found to be 6.6-26.2% in this study. Prevalence of manifestations of non skeletal fluorosis was found to be 25% to 40%. 40 -60% of school children were found to be suffering from Dental fluorosis in the study area. Withdrawal of source(s) identified for fluoride by supplying domestic and community filters along with dietary intervention leads to decreased manifestations of the three types of fluorosis but from the study it was evident that only 20-40% of population were using domestic filters due to lack of awareness regarding health hazards of Fluoride toxicity, lack of maintenance and delay in repair of parts and lack of monitoring and supervision.
Conclusion:
More extensive studies involving large group of population may be needed in future to measure the impact. Supply of safe water with nutritional interventions based on the above findings may be necessary to combat the problem of fluorosis.
Keywords
Fluoride
Fluoride toxicity
Domestic filters
INTRODUCTION
Fluoride is one of the important factors in water quality management due to its adverse health effects. The problem of high fluoride concentration in groundwater resources has become one of the most important toxicological and geo-environmental issues in India. Excessive fluoride in drinking water causes dental and skeletal fluorosis, which is encountered in endemic proportions in several parts of the world. [1] World Health Organization (WHO) guideline value and the permissible limit of fluoride as per Bureau of Indian Standard (BIS) is 1.5 mg/L. [2]About 20 out of 35 states and union territories of India were identified as endemic for fluorosis [3] and about 66 million people in these regions are at risk of fluoride contamination. Fluorosis is known to occur due to the entry of excess fluoride into the body. It is a slow, progressive, crippling malady that affects every organ, tissue, and cells in the body, and results in health complaints that overlap with several other disorders. Most of the fluorides are readily soluble in water. Prolonged ingestion of fluoride above permissible level through water is the major cause of fluorosis.
Fluorosis disease can occur in three forms: dental fluorosis, skeletal fluorosis and non-skeletal fluorosis. Dental fluorosis occurs in the permanent teeth in children after 8 years of age.[3][4] Skeletal fluorosis affects the bones and major joints of the body. [5][6] Non-skeletal fluorosis affects invariably all the soft tissues, organs, and systems of the body. [7] Dental fluorosis is a good indicator of exposure to excessive amounts of fluoride. The main natural source of inorganic fluorides in soil is the parent rock. Fluoride can also enter the body through food and fluoridated dental products as well as drugs. To confirm diagnosis of fluorosis, the fluoride is mainly estimated in serum, drinking water, and urine. [7]10-40% districts are affected in Assam, Jammu & Kashmir, Kerala, Chattisgarh and West Bengal. [8] In West Bengal, fluoride was first detected at Bhubanandapur in Nalhati I block of Birbhum district in 1996. During a rapid assessment survey by Public Health Engineering Department, Government of West Bengal (2005), 729 sources were found to be contaminated with fluoride above 1.5 ppm in 43 blocks of seven districts of West Bengal, with the affected population being approximately 2.26 lakhs. Fluoride level in West Bengal varies from 1.1 to 4.47 mg/L. [9] Studies show that withdrawal of sources identified for fluoride often leads to reduction of fluoride in the body fluids (re-testing urine and serum after a week or 10 days) and results in the disappearance of non-skeletal fluorosis within a short duration of 10-15 days. [7]
Fluorosis is an impending public health problem in West Bengal affecting a large number of population, and Birbhum is one of the affected districts with seven affected blocks. The present study was conducted to see the extent of fluorosis in two selected affected blocks of Birbhum District of West Bengal and to determine the pattern of usage of domestic filters by the villagers of the above selected endemic villages.
Objectives:
To determine the prevalence of signs and symptoms of suspected Dental, Skeletal and non skeletal fluorosis along with their food habits, addictions and use of fluoride containing toothpaste among participants taking water with fluoride concentration above permissible limit in the two selected affected blocks of Birbhum District of West Bengal.
To determine the pattern of usage of domestic filters by the villagers of the above selected endemic villages
Methodology
Seven blocks of Birbhum district of West Bengal were endemic for fluorosis. Out of these seven blocks, two blocks Rampurhat I and Khoerasol were selected randomly for the study. Within Rampurhat Block I, two affected villages, i.e. Junitpur and Kamdevpur, [with the fluoride content in their tube wells varying from 2.6 to 11 mg/L (PHED report 2008)] and within Khoerashol block three villages i.e. Fullarchak, Baruipara and Jamrand village [with the fluoride content in their tube wells varying from 2.6 to 4 mg/L (PHED report 2008)] were selected for the study. 10 families in Junitpur and Kamdebpur in Rampurhat Block and 20 families in Fullarchak, Baruipara and Jamrand village of Khoerashol Block i.e a total 30 families were selected randomly out of families having past history of taking water from an unsafe source (a tube well having fluoride concentration higher than the permissible level) in these two blocks. Out of these 30 families a total 125 family members, 45 from Junitpur and Kamdebpur villages of Rampurhat Block and 80 from Fullarchak, Baruipara and Jamrand village of Khoerasol Block were finally inter viewed and examined for health survey. A total 60 school children (30 in Jamrand Primary school in Jamrand village and 30 in Chakatla primary school in Kamdevpur village) were examined and screened for Dental fluorosis. All these families and the primary schools were supplied domestic filters for removal of fluoride.
All the selected families had a past history of taking water from an unsafe source (a tube well having fluoride concentration higher than the permissible level) situated nearby before using the water from the domestic filters. The selected families were visited during the study period (November- December 2012) for inspection of domestic filters and interview and clinical examination of family members taking water from those filters. The objective of the visit is for identification, treatment and motivation of persons suffering from adverse health effects of Fluoride toxicity. The condition, status and functioning of Domestic Filters supplied to villagers were also studied along with the acceptability of filters as a drinking and cooking water source by the villagers. The perception of the villagers about the filter water was also noted.
The families who are not using the filter were also studied to record the reasons for not using the filters.
Two primary schools were also visited to screen fluorosis patients from the school children of the above schools and to observe the functioning status of filters supplied to them.
After taking consent and explaining the purpose of the visit, the family members of selected families along with the school children were interviewed regarding presence or absence of various signs and symptoms of dental, skeletal and non skeletal fluorosis, addictions, diet, food habits, use of fluoride containing toothpaste etc and clinically examined for identification of signs and symptoms of suspected Dental, Skeletal and non skeletal fluorosis.
Enquiries were also made regarding presence and absence of any difficulties in using the supplied Domestic filters and their satisfaction level and the user friendliness of the filters. Water was also collected from the filters for chemical and the bacteriological testing and the families having some difficulties in using the filters were explained regarding the ways to overcome such difficulties after proper inspection Counseling, advice and treatment of minor ailments were also given to family members and the school children. The importance of using the domestic filter also explained to them.
Ethical clearance was obtained prior to the initiation of the study.
Dental fluorosis, skeletal fluorosis, and non-skeletal fluorosis were assessed by case definitions and diagnostic criteria developed by Fluorosis Research and Rural Development Foundation, New Delhi[3],[5] ,[7] Data collected were analyzed by suitable statistical methods.
RESULTS
44.4% and 47.5% of the study population are found to be suffering from Dental fluorosis in Rampurhat and Khoerasol Block (Table I and Fig I)
| Disease Manifestations |
Rampurhat Block (n=45) Prevalence on Nov - Dec 2012 No (%) |
Khoerasol Block (n=80) Prevalence on Nov-Dec 2012 No (%) |
|---|---|---|
| Dental Fluorosis | 20 (44.4) | 38 (47.5) |
|
Lactating / Pregnant mothers |
1 | 2 |
| Abortion/Still Births | 1 (2.2) | 2 (2.5) |
| Skeletal Fluorosis | ||
| a) Touch the chin with the chest (inability) |
10 (22.2) | 21 (26.2) |
| b) Bend to touch the toes (inability) |
7 (15.5) | 16 (20.0) |
| c) Stretches arm to touch the back of the head (inability) |
3 (6.6) | 12 (15.0) |
|
NonSkeletal Fluorosis |
- | |
| a) Pain in the stomach | 9 (20.0) | 20 (25.0) |
| b) Bloating or flatulence |
11 (24.4) | 22 (27.5) |
| c) Loss of appetite | 9 (20.0) | 24 (30.0) |
| d) Constipation followed by diarrhoea |
5 (11.1) | 10 (12.5) |
| e) Polyurea/ Polydypsia |
15 (33.3) | 32 (40.0) |
| f)Fatigue/Depression | 12 (26.6) | 25 (31.2) |
| g) Muscle weakness | 3 (6.6) | 7 (8.7) |
| Fluoride Toothpaste | 28 (62.2) | 41 (51.2) |
| Consumption of food | ||
| a) Supari | 4 (8.8) | 8 (10.0) |
| b) Tobacco | 7 (15.5) | 15 (18.7) |
| c) Black lemon tea | 28 (62.2) | 52 (65.0) |
| d) Black rock salt | Nil (0) | Nil (0) |
| e)Adequate intake of Fruits & Vegetables |
23 (51.1) | 45 (56.2) |
| f)Adequate intake of Fish |
19 (42.2) | 42 (52.5) |
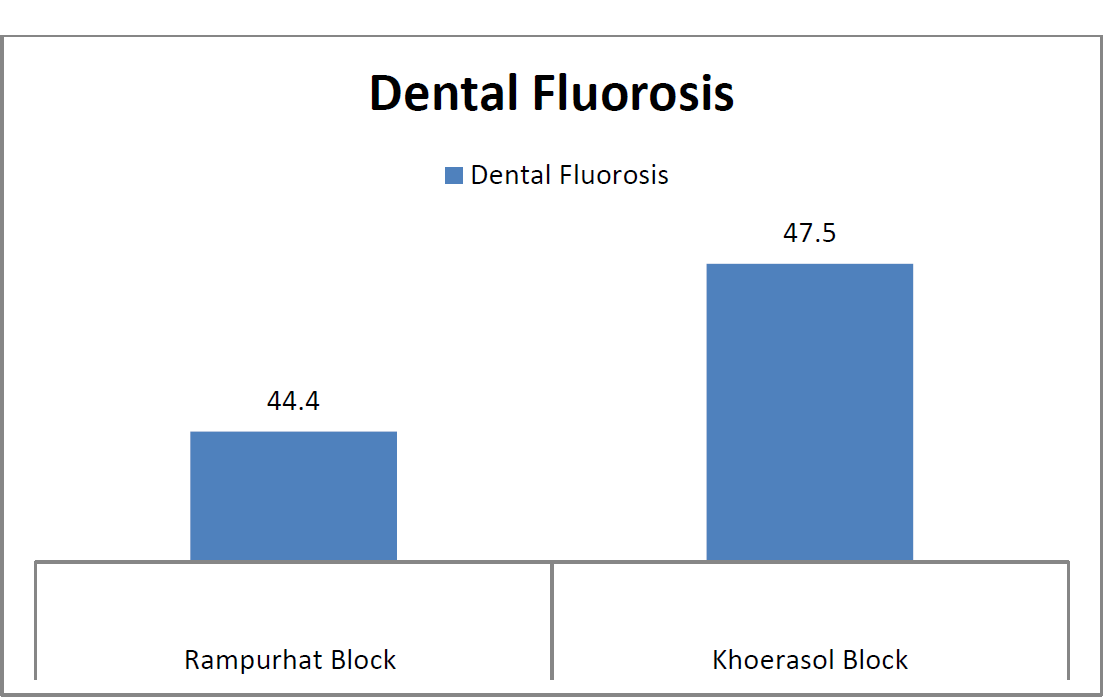
- Graphical presentation of signs of Dental fluorosis in percentage among the participants in Rampurhat Block and Khoerasol Block
Most common sign among skeletal fluorosis being inability to touch the chin with chest (22.2%& 26.2%) followed by inability to touch the toes without bending the knees (15.5% & 20%) and inability to stretch the arm to touch the back of the head (6.6% & 15%) among study population in Rampurhat and Khoerashol Block (Table I and Fig 2).
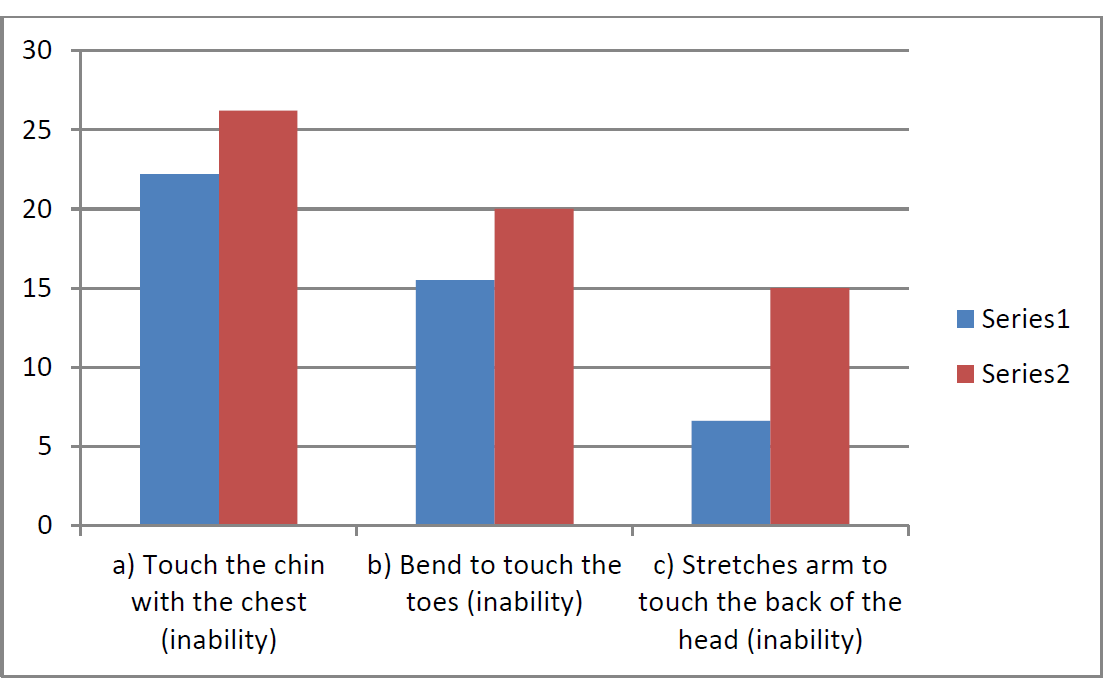
- Graphical presentation of signs of skeletal fluorosis in percentage among the participants Series 1- Rampurhat Block, Series 2 - Khoerasol Block
Polyurea/Polydypsia (33.3% & 40%), fatigue or depressions (26.6% & 31.2%) followed by bloating or flatulence (24.4%& 27.5%), loss of appetite (20% & 30%) and pain in stomach (20% &25%) were common among non skeletal fluorosis symptoms (Table I and Fig 3).
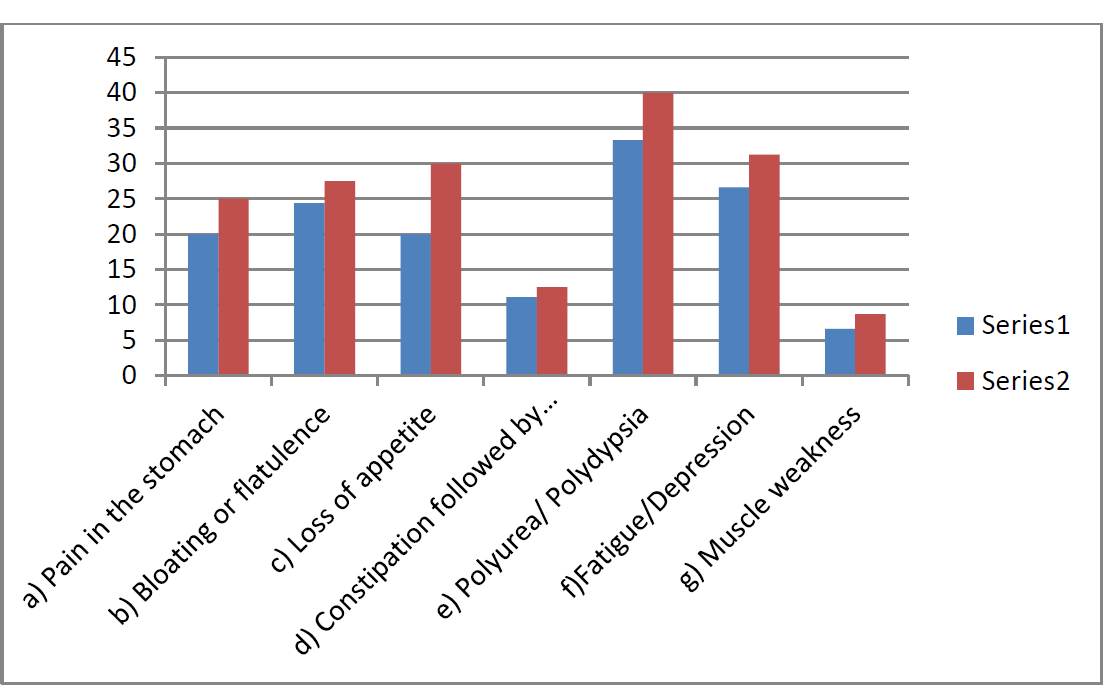
- Graphical presentation of symptoms of non skeletal fluorosis in percentage among the participants. Series 1- Rampurhat Block, Series 2 - Khoerasol Block
62.2% and 51.2% of the study population still using fluoride containing toothpaste in Rampurhat and Khoerashol Block (Table I). A large number of population in Khoerasol block are using tobacco (Guraku) and ash as an alternative to tooth paste. 62.2% and 65.0% of study population drink black lemon tea containing high fluoride in Rampurhat and Khoerashol Block (Table I and Fig 4) as milk is not easily available and even if it is available the villagers cannot afford it. Only those families having cow or buffalo in their house take milk tea.51.1% and 56.2% of study population takes plenty of green leafy vegetables and fruits containing antioxidants in Rampurhat and Khoerashol Block (Table I and Fig 4).42.2% and 52.5% of study population take adequate amount of fish followed by less frequent amount of egg and meat in Rampurhat and Khoerashol Block (Table I and Fig 4).
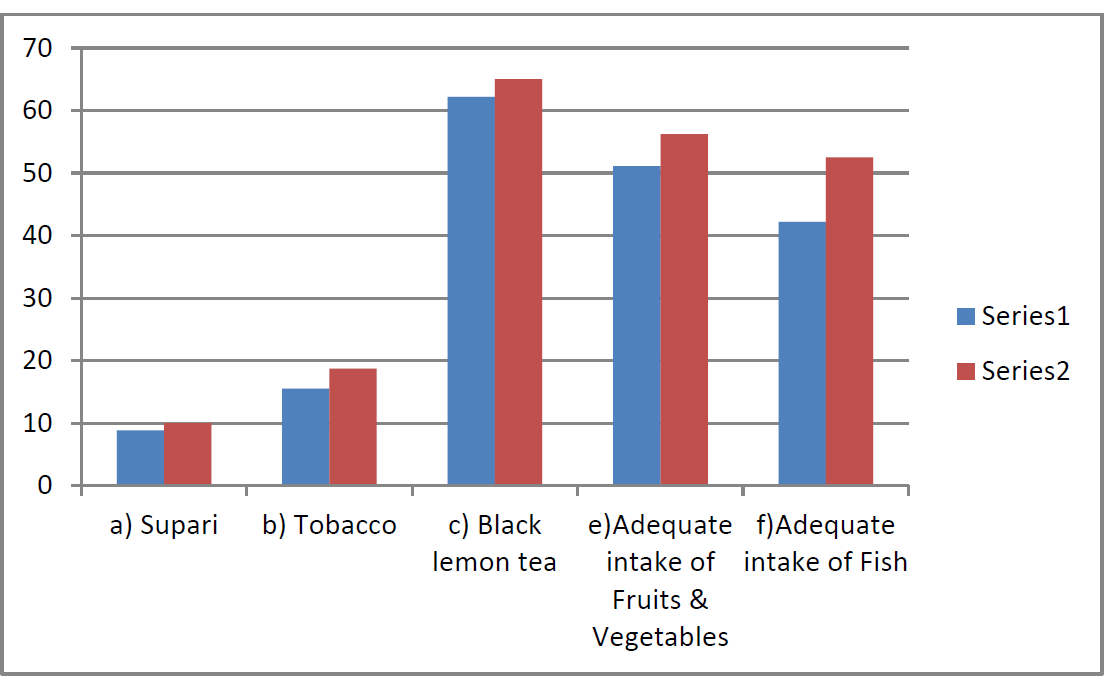
- Graphical presentation of dietary intake in percentage among the participants. Series 1- Rampurhat Block, Series 2 - Khoerasol Block
In general if we compare the manifestations of fluorosis among the study population in the two blocks, the condition of patients in Khoerasol Block (specially in Fullarchak village) is worse compared to patients in Rampurhat Block.
The children of Jamrand Primary school in Jamrand village of Khoerasol Block and Chakatla primary school in Kamdevpur village of Rampurhat Block were examined and screened for Dental caries and around 40% children in Jamrand Primary school and 30% children in Chakatla primary school were found to be having signs of dental fluorosis (60%- mild and 40%- Mod). Majority of school children suffering from Dental fluorosis were found to be from Fullarchak village.
The filter installed in the school was found to be unutilized and the children were seen drinking water from unsafe sources like the school tube well in Jamrand primary school and nearby tubewell in Chakatla School.
Status of utilization of Domestic filters
40% of selected families in Junitpur and Kamdevpur villages in Rampurhat Block are using domestic filters. Whereas only 20% of selected families in Fullarchak village, 10% of selected families in Baruipara village and 25% of selected families in Jamrand village of Khoerashol block are using domestic filters and prevalence of manifestations of fluorosis is more in Khoerasol block in comparison to Rampurhat block. 60% of selected families in Jamrand and Baruipara village are using river water in the filter instead of tube well water as large number of families in these two villages use river water for drinking and cooking purposes and some families use pond water for cooking purpose for a long time since their stay in the above villages.So the basic purpose of supplying Fluoride removing filters to the above families was not served. Water after back washing is disposed indiscriminately by the families in Khoerasol Block as they have no idea of proper disposal.
Many families are cleaning the candle filters with soap water, detergent etc instead of scrubbing. A large number of families are not aware of the health hazards of drinking water containing high level of Fluoride in Jamrand and Baruipara villages and their felt needs were not assessed before supplying the filters so they have separated the individual parts of the filter and using them for other purposes like children toys, flower pots, sitting stools etc.
Lack of use of domestic filters along with lack of awareness is the main causes of increase in prevalence of all types of fluorosis in Khoerasol block in comparison to Rampurhat block.
Discussion
The overall prevalence of dental fluorosis among the study participants was found to be 44.4-47.5% in this study. Choubisa in his study conducted in southern Rajasthan found the overall prevalence of dental fluorosis to be 45.7%. [10] Bharati et al., in their study conducted in Gudag and Bagalkot districts of Karnataka, found the prevalence of dental fluorosis to be 35%. [11] Yellowish-brown discoloration of teeth with horizontal streaks was the most common symptom of dental fluorosis, followed by blackening/pitting/chipping of teeth. Bharati et al. reported browning of teeth in 64.29% and pitting of teeth in 32.4% subjects. [11]Similar positive correlation between fluoride concentration and Dental Fluorosis Index (DFI) score was also found in studies by Ruan et al., [12] Mann et al., [13] Acharya, [14] and Kumar. [15]
Prevalence of manifestations of skeletal fluorosis was found to be 6.6-26.2% in this study. Bharati et al., in their study performed in Gudag and Bagalkot districts of Karnataka, found the prevalence of skeletal fluorosis to be 17% and both types to be 12.67%. [11] Choubisa in his study conducted in southern Rajasthan found that the overall prevalence of skeletal fluorosis was 22%. [10]The most common sign among skeletal fluorosis patients was found to be inability to touch the chin with chest (22.2% and26.2%, respectively) followed by inability to bend to touch the toe (15.5 to 20%). Joint pain was found in 31.87% subjects in the study done by Bharati et al. [11] Narayana et al. reported joint pain and neck stiffness in 50-70% of cases. [16] Shashi et al., in their study conducted in three endemic areas of Punjab state, observed back pain (73%) and neck pain (34%) as the symptoms of skeletal fluorosis.[17]
In the present study, tobacco consumption in any form was found in 15.5-18.7% of the subjects. Kubakaddi et al. observed that 40% of the tobacco chewers were suffering from dental and skeletal fluorosis[18] It is evident from previous studies that withdrawal of source(s) identified for fluoride leads to reduction of fluoride in body fluids and shall result in disappearance of health problems emanating from non-skeletal fluorosis within a short period.[9]
Although the description of disease was done long back by eminent physicians like Dr S.S.Jolly, Dr Amaijeet Sing and Dr C.G.Pandit19 indicating a disease entity that originated in India in early 1930, not much have been done till date regarding its mitigation measures. However in to address the problem of fluorosis in the country, National Programme for Prevention and Control of fluorosis was launched in 2008-09 with an objective to collect, assess and use the baseline survey data of Department of Drinking Water Supply for Fluoride mapping along with comprehensive management and capacity building.20,21
Conclusion
It is evident from this study that fluorosis is a definite public health problem in the selected block of Birbhum district, with increased prevalence of dental, skeletal, and non-skeletal fluorosis found among the study population. Withdrawal of source(s) identified for fluoride by supplying domestic and community filters along with dietary intervention leads to decreased manifestations of the three types of fluorosis 22 but from the study it is evident that 40% of selected families in Junitpur and Kamdevpur villages in Rampurhat Block and 10 -25% of selected families in Khoerashol block are using domestic filters and prevalence of manifestations of fluorosis is more in Khoerasol block in comparison to Rampurhat block. The reasons for not using the domestic filters are due to lack of awareness regarding health hazards of Fluoride toxicity, lack of maintenance and delay in repair of parts and lack of monitoring and supervision. Only supply of filters will not solve the problem but supply of safe water, awareness generation, motivation, demand generation for domestic filters along with nutritional interventions based on the above findings may be necessary to combat the problem of fluorosis.
Acknowledgement
The author gratefully acknowledges the financial support provided by UNICEF, Kolkata. Support and cooperation rendered by Mr. S. N. Dave, WES specialist, UNICEF, Kolkata, Mr. Sundarraj, Consultant, WES, UNICEF, Kolkata, and Prof. Anirban Gupta, Professor, Department of Civil Engineering, BESU, Howrah, to conduct the study is hereby acknowledged.
References
- Human health effects: Fluoride in drinking water WHO drinking -water quality series. London: IWA Publishers; 2006. p. :29-35.
- [Google Scholar]
- Chemical aspects. W.H.O. Guidelines for drinking- water quality. In: W H O. Vol 1. (3rd). Geneva: W.H.O.; 2004. p. :184-6.
- [Google Scholar]
- Prevention and control of fluorosis: Dental fluorosis- symptoms. (1st). New Delhi: National Technology Mission on Drinking Water; 1991. p. :7-9.
- [Google Scholar]
- Prevention and control of fluorosis- health aspects. In: Oral cavity, teeth and dental fluorosis. Vol 1. New Delhi: Rajiv Gandhi National Drinking Water Mission, New Delhi: Ministry of Rural development; 1994. p. :53-7.
- [Google Scholar]
- Prevention and control of fluorosis: Skeletal fluorosis- symptoms. (1st). New Delhi: National Technology Mission on Drinking Water; 1991. p. :4-6.
- [Google Scholar]
- Prevention and control of fluorosis- health aspects vol. 1: Effects of fluoride on the bones, the skeletal system & skeletal fluorosis. New Delhi: Rajiv Gandhi National Drinking Water Mission, New Delhi: Ministry of Rural development; 1994. p. :40-9.
- [Google Scholar]
- Fluorosis: An easily preventable disease through practice and intervention. New Delhi: Fluorosis Research & Rural Development Foundation; 2005. p. :10.
- [Google Scholar]
- [home page on Internet].New Delhi: Fluorosis Research and Rural Development Foundation online resource. Available from: http://www.fluorideandfluorosis.com/fluorosis/districts.html (accessed )
- [Google Scholar]
- [Internet].New Delhi: Fluorosis Research And Rural Development Foundation online resource. Available from: http://www.fluorideandfluorosis.com/fluorosis/prevalence.html (accessed )
- [Google Scholar]
- Clinical symptoms of dental and skeletal fluorosis in Gadag and Bagalkot districts of Karnataka. J Hum Ecol. 2005;18:105-7.
- [CrossRef] [Google Scholar]
- Dental fluorosis and dental caries in permanent teeth: Rural school children in high fluoride areas in the Shaanxi province, China. Acta Odontol Scand. 2005;63:258-65.
- [CrossRef] [PubMed] [Google Scholar]
- Fluorosis and caries prevalence in a community drinking above optimal fluoridated water. Community Dent Oral Epidemiol. 1987;15
- [CrossRef] [PubMed] [Google Scholar]
- Dental caries, its surface susceptibility and dental fluorosis in South India. Int Dent J. 2005;55:359-64.
- [CrossRef] [PubMed] [Google Scholar]
- Intra-oral distribution of dental fluorosis in Newburgh and Kingston, New York. J Dent Res. 2000;79:1508-13.
- [CrossRef] [PubMed] [Google Scholar]
- Mitigation of fluorosis in Nalgonda district villages: 4 th International workshop on fluorosis prevention and defluoridation of water. 2004 Available from: http://www.de-fluoride.net/4th proceedings/98-106.pdf (accessed )
- [Google Scholar]
- Incidence of skeletal deformities in endemic fluorosis. Trop Doct. 2008;38:231.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of fluoride rich food adjuncts and prevalence of fluorosis. J Hum Ecol. 2005;17:43.
- [CrossRef] [Google Scholar]
- Epidemiological, clinical and biochemical study of endemic dental and skeletal fluorosis in Punjab. Brit.Med.J.. ;4:427-1968.
- [CrossRef] [PubMed] [Google Scholar]
- “Health impact of supplying safe drinking water on patients having various clinical manifestations of Fluorosis in a endemic village of West Bengal”. Journal of Family Medicine and Primary Care. 2013;2(1):74-78.
- [Google Scholar]






