Translate this page into:
Occupational Stress among Medical Practitioners in Gandhinagar City, Gujarat: A Cross-sectional Study
Corresponding author: Dr. Anish Kumar Sinha, Institute of Public Health Gandhinagar, Opp. Air Force Headquarter, Nr Lekawada Bus Stand, Lekawada, Gandhinagar 382042, E-mail: asinha@iiphg.org
How to cite this article: Sinha AK, Pandya AK, Pingle S. Occupational Stress among Medical Practitioners in Gandhinagar City, Gujarat: A Cross-sectional Study. J Comprehensive Health 2020;8(2): 55-59.
Abstract
Introduction:
It is well established that medical practitioners experience high levels of job stress. This study assessed the perceived stress and stressors among medical practitioners from various specialities in Gandhinagar City of the Gujarat State.
Materials and Methods:
Using a cross-sectional research design, 72 medical practitioners, from different specialities and practice settings in Gandhinagar City of the Gujarat State, were briefly interviewed using the semistructured interview protocol and Perceived Stress Scale (PSS), during the period from May to June 2019.
Results:
The study showed that the majority of medical practitioners had a moderate level of stress (70%), and 11% of them had a severe level of stress. A chi-square test of independence revealed that gender (p=.0029), speciality (p=.0021), practice setting (p=.021), and experience (p=.001) were statistically significant for stress levels. Further, the average PSS score differed significantly according to stressors, namely, work related (p=.004), financial (p=.008), family (p=.049), excessive workload (p=.001), night duty (p=.012) and long working hours (p=.000). However, most medical practitioners did not perceive stress as a problem, and perhaps for that reason necessary actions for stress management were not reported by them.
Conclusion:
Present study reported high level of stress among medical practitioners, indicating a critical need to address occupational stress among medical practitioners in Gandhinagar City. Immediate actions are warranted for preventing adverse effect of stress on overall health and wellbeing of medical practitioners. Future study on a large sample that assesses stress, mental health risk, and coping responses would be important step.
Keywords
Medical practitioners
doctors
occupational stress
perceived stress scale
Gandhinagar city
Gujarat
India.
Introduction:
It is well acknowledged that medical professionals experience a high level of stress when occupational demands exceed their ability to cope.[1-2] In the recent past, increased incidence of stress-induced disorders among professionals from medical occupation[3-4] have been reported. Many studies in the west have identified stress as a factor in poor job performance, low job satisfaction, physical and mental health problems among health professionals including medical practitioners (doctors from different specialities).[5-9] The quality of health care can be extremely influenced by the stress among medical practitioners. Stress has been found to be associated with lapses inpatient care.[7-10] Long hours, large numbers of patients, and sleep deprivation have been recognised as risk factors for stress among medical practitioners.[8,9] When the level of stress exceeds a critical level, it can manifest as psychological distress, burnout and increases a risk of physical ailments such as hypertention, diabetes, heart disease and so[10]. Studies on stress and its impact among medical practitioners conducted in India are largely among different sets or subsets of medical specialities. Moreover, studies in Western India, particularly in Gujarat are limited. Therefore, this study was conducted with an aim to assess perceived stress and potential stressors among medical practitioners from different medical specialities and practice settings in Gujarat.
Materials and Methods:
A cross-sectional research design was used for the study. Considering time constraint and operational feasibility, convenient sampling was opted for the data collection. Out of 465 medical practitioners registered with Indian Medical Association-Gandhinagar District Chapter, total 72 medical practitioners from Gandhinagar City representing different specialities and practice settings participated in the study. They were interviewed using semi-structure brief interview protocol and investigator (first author) filled participants' resoponses on the Perceived Stress Scale (PSS),[11] during the period from May to June 2019. The PSS is reliable and validated tool, having an internal consistency of 0.85 (Cronbach Alpha). It primarily assesses the degree to which participants evaluate their lives as stressful during the past month.[11]
Semi-structured brief interview was used to gather information related to demographic profile, speciality, their perspectives on stress management while PSS was used to assess level of stress in past one month. Both tools were pilot- tested with 10 representative sample before actual study and these data were not included in the final data sets of the study. Tools were refined based on pilot-testing. PSS scores ranged from 0 to 40 with higher scores indicating higher perceived stress. The PSS score was calculated by summing up the scores of all respondents. As per the manual of the scale, scores ranged from 0-13 was considered low stress, scores between 14-26 was considered moderate stress and scores ranging from 27-40 was considered severe stress.[11] Data were entered in Microsoft Office spread-sheet for the analysis and exported to Statistical Package for the Social Sciences version 14 for statistical analysis. Considering the categorical varibales, chi-square test was applied to examine the association of stress with socio-demographic variables such as speciality, years of experience, practice sector, gender and so. Pearson's Correlation either P < 0.01 or P<0.05 was considered to be statistically significant.
Ethical Considerations:
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institution and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Results:
Results are classified in three sections, i.e. characteristics of the study participants, perceived stress & stressors and medical practitioners' perspectives on stress and its management.
Section I: Characteristics of the study participants
Majority of medical practitioners included Family Physician (MBBS) (17.1%), Obstetricians & Gynaecologists (16.3%), Paediatricians (15.6%), Physician (13.2%), Emergency Medicine specialist (9.3%), General Surgeon (11.5%), Ophthalmologist (7.2%). Other medical professionals were orthopaedic, critical care specialist, chest and TB specialist, ENT specialist, neurosurgeon, pathologist, and radiologist (1.4% each).
Mean (SD) age of participants was 39.52 (± 2.08). Slightly more than half of the participants (53%) belonged to age group 40 to 60 years, followed by 20-40 years' age group (47%). The proportion of males were 74 % and 26% were females.
In terms of practice settings, about three-fourth (74%) worked in private sector, either having their own hospital or working in private multi-speciality or corporate hospital; more than a quarter (26%) were from Government sector and one practitioner was from Trust hospital. More than half (59%) medical practitioners were having experience between 5 to 20 years followed by 30% between 1 to 5 years, and 11% were practicing for more than 20 years.
Section II: Perceived Stress and Stressors
The mean of the PSS scores was 24. The study showed that the majority of medical practitioners had a moderate level of stress (70%), and 11% of the medical practitioners had a severe level of stress. The average PSS scores, according to sociodemographic and work characteristics, are shown in Table 1. The average PSS score differed significantly according to gender, specialty, years of experience, and practice settings.
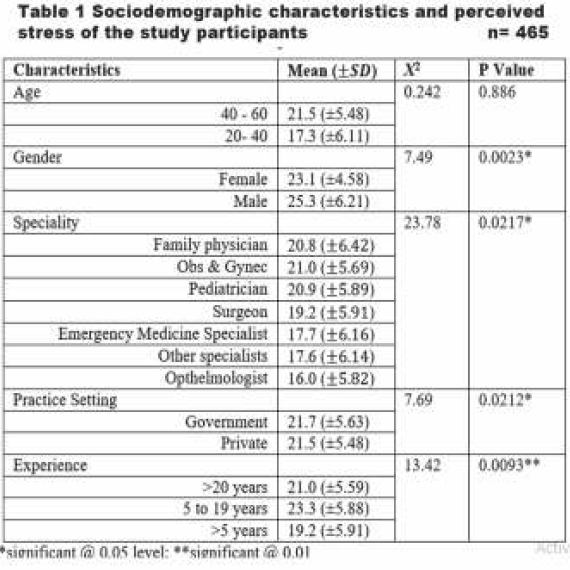
Gender, speciality, practice setting, and experience were emerged as statistically significant for stress levels. A chi- square test of independence was performed to examine the relationship between gender and stress, which was significant at 0.5 level, X2 (1, N = 72) = 8.9, p = .0029 . Female medical practitioners had a higher proportion of moderate (79%) and severe (16%) stress compared to stress levels, moderate (66%) and severe (9%) stress, among males. Speciality was also appeared significant at 0.5 level, X2 (12, N = 72) = 23.78, p = 0.0217.
Amongst specialities, family physician (M=20.8), Obs. & Gynec. (M=21.0), Pediatrician (M=20.9) and Surgeon (M=19.2) had higher mean compared to other specialities. Private sector medical practitioners had more stress compared to medical practitioners working with the Government sector and significant association was found, X2 (2, N = 72) = 7.69, p =0.021.
Medical practitioners with less than 20 years of practice experience had experienced moderate (25) stress while medical practitioners with less than 5 years had moderate (27.8%) and severe (4.2%) stress compared to medical practitioners with more than 20 years of practice. Significant association between years of experience and stress was found, X2 (4, N = 72) = 13.42, (p < 0.001).
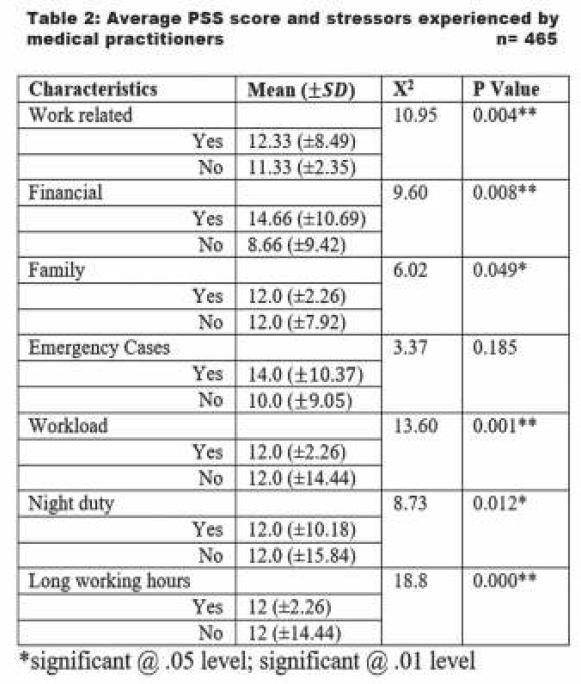
Table 2 shows the average PSS score according to stressors experienced by medical practitioners. The average PSS score differed significantly according to stressors, namely, work related (p=.004), financial (p=.008), family (p=.049), excessive workload (p.=.001), night duty (p.=.012) and long working hours (p.=.000). No significant association between emergency cases and stress was reported.
Section III: Medical Practitioners' Perspectives on Stress and its Management
During the last month preceding the survey, 75% of the medical practitioners often felt stressed, 43% of them felt upset because of unexpected events, 46% felt angered by circumstances that were beyond their control, 38% felt unable to control important things in their life, and 33% experienced that these difficulties were piling up, which were too demanding and overwhelming. In contrast, 25% of the medical practitioners reported that things were going their way, 18% had often been able to control things in their life, and 15% felt confident in their ability to handle personal problems.
Work-life balance emerged as the greatest challenge among medical practitioners. Many medical practitioners (76%) pointed out work related stress caused by workload, competition in the market, loan repayment, and long work hours influenced their personal life greatly and were not able to spare quality time with family. In terms of practice settings, medical practitioners from private setting (83%, n=52) expressed competition, uncertainity of the market, long working hours and inability to spare time with family were cited more frequently as stressors while medical practitioners from public sector (73%, n=20) highlighted dissatisfaction with work environment, excessive work load, night duty as stressors.
Despite acknowledging the stressors, most of them (94%) did not perceive stress as a problem, which is contradictory to the study findings. It indicates denial of the problem and may impact their ability to use coping strategies. Many medical practitioners (63%) reported dealing with routine stressors by engaging in emotional withdrawal (bottling up emotions), social isolation (disconnecting with others), unhealthy eating (eating junk food), and substance use (more commonly, cigarrete & alcohol). These invariably predispose them to the risk of poor physical and mental health.
Discussion:
Stress is a common experience among healthcare workers. It is well acknowledged that medical practitioners experience higher levels of stress and stress-related health problems than other occupational groups[12,13]. The study showed that the mean PSS score reported in the study was 24, which indicated moderate perceived stress. The majority of medical practitioners had moderate stress (73%), and 18% of them reported severe stress. This finding is comparable with other study outcomes in India and other countries. For example, one study reported a mean of 23.45 among 31 medical officers in Kerala; another study conducted in Tamil Nadu with 84 doctors working in a tertiary care hospital reported a mean of 18.3.[14-15] Similar results were reported in the study conducted in Canada, Saudi Arabia, and Jordan.[16-18]
The presence of stress is associated with speciality, practice setting (Govt Vs. Private), years of experience and gender. In the present study, stress was significantly associated with specialities such as surgery, obstetrics and gynacology, medicine, and pediatrics. It is a well-known fact that the obstetrics and gynacology has the highest prevalence of stress and burnout among all specialities.[10,16,19] These specialities are characterized by sleep deprivation, long weekly working hours, clinical responsibilities, and issues related to Insurance crises.[16] In terms of practice settings, private medical practioners experienced a higher stress level as compared to those in public sector. This finding is similar to the study conducted in Malasia, India and Ethiopia.[20-24] Furthermore, the present study also revealed that years of experience had significant relationship with the experience of stress; medical practitioners with less than 10 years reported higher stress level compared to experienced practitioners. The study conducted in Saudi Arabia indicated similar findings, younger medical practitioners (with less years of experience) reported higher level of stress.[18]
Gender difference in stress was quite evident from the present study as well as available literature. Female medical practioners had a significantly higher level of stress than male counterpart. Several studies are in agreement with this finding[10,14,15,25]. The reasons for this difference may be because women are endowed with dual responsibilities of career and family that add additional stressors to their occupation. Eexcessive work, long duty hours, night duty have been recognized as potential stressors.[17,26,27] Present study echoed the same. Stress negatively impacts work performance and patient care, including medication errors, suboptimal care, and patient dissatisfaction.[7,8,19] Moreover, it adversely impacts overall psychological and physical health of a person.
In the present study, medical practitioners denied the problems which is worrisome. Recent study conducted with medical officers in Kerala[15] reported denial and substance use as coping response to the stress. Thus, periodic selfassessment of stress, learning coping strategies and seeking professional help from psychologists whenever needed are essential preventive measures. Recent systematic reviews and mata-analyses on preventive stress management interventions were found to be effective in reducing stress and quality of life of medical practitioners. [28-29] Physical exercise, sports, and de-stressing techniques like listening to music were significant in coping with occupational stress.[30] Such coping strategies can play vital role in effectively dealing with occupational stress. Professional bodies like Indian Medical Association can play a crucial role in creating awareness as well as incorporating short-term courses on yoga, stress management, work-life management, etc as part of continuing medical education.
The strength of the study includes the fact that it is a first attempt to understand the perceived stress and stressors among the medical practitioners from various specialities in Gandhinagar City. However, the results need to be interpreted with caution due to small sample size and the cross-sectional nature of the study. Future study on a large sample can assess stress, its impact on physical and mental health, coping responses as well as can explore available resources including psychological services for stress management. Prospective studies may also examine the predictive validity of the stress and coping responses over a period of time.
Conclusion:
Medical practitioners across various specialities and practice settings in Gandhinagar City experience moderate to severe stress. Significant stressors were work-related stressors, family-related stressors, and excessive work load, late working hours and night duty. Although study findings cannot be generalized due to restricted sample size, the study results highlight a critical need to address occupational stress experienced by medical practitioners.
Conflict of Interest:
None
Funding Source:
None
References:
- Stress in health professionals: Psychological and Organizational Causes and Interventions. 2000.
- [Google Scholar]
- Role Stress among doctors. Journal of Health Management. 2005;7(1):151-156.
- [CrossRef] [Google Scholar]
- Work-related stress among health professionals in northern Jordan. Occupational Medicine. 2012;62(2):145-147.
- [CrossRef] [PubMed] [Google Scholar]
- Risk of affective and stress related disorders among employees in human service professions. Occup Environ Med. 2006;63(5):314-9.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of common mental disorders among hospital physicians and their association with self-reported workability: a cross-sectional study. BMC Health Services Research. 2012;12(1):292.
- [CrossRef] [PubMed] [Google Scholar]
- Stress and disorders of the stress system. Nature Reviews Endocrinology. 2009;5(7):374.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological problems and burnout among medical professionals of a tertiary care hospital of North India: A cross-sectional study. Indian Journal Psychiatry. 2018;0(2):175-188.
- [CrossRef] [PubMed] [Google Scholar]
- Emotional intelligence, perceived stress and burnout among resident doctors: an assessment of the relationship. National Medical Journal of India. 2013;26(4):210-3.
- [Google Scholar]
- Prevalence of stress among resident doctors working in Medical Colleges of Delhi. Indian Journal of Public Health. 2010;54:219-23.
- [CrossRef] [PubMed] [Google Scholar]
- Stress levels of critical care doctors in India: A national survey. Indian Journal of Critical Care Medicine. 2015;19(5):257-64.
- [CrossRef] [PubMed] [Google Scholar]
- Perceived stress scale. Measuring stress: A guide for health and social scientists. . 1994;10:235-283.
- [Google Scholar]
- Perceived stress effects among Doctors exposed to surgical source of stress, 1. Stress Research and Stress Management. 2001;1:1-3.
- [Google Scholar]
- Perceived stress and psychological distress among Chinese physicians: The mediating role of coping style. Medicine. 2019;98(23)
- [CrossRef] [PubMed] [Google Scholar]
- Perceived stress levels and its sources among doctors and nurses working in a tertiary care teaching hospital, Kancheepuram, Tamil Nadu. National Journal of Community Medicine. 2016;7(7):603-608.
- [Google Scholar]
- Stress and coping among medical officers in Kerala: a cross-sectional study. Kerala Journal of Psychiatry. 2017;30(2):79-83. DOI: 10.30834/KJP.30.2.2018.13
- [CrossRef] [Google Scholar]
- Stress and coping among medical officers in Kerala: a cross-sectional study. Kerala Journal of Psychiatry. 2017;30(2):79-83. DOI: 10.30834/KJP.30.2.2018.13
- [Google Scholar]
- Perceived Stress Among Resident Doctors in Jordanian Teaching Hospitals: Cross-Sectional Study. JMIR Public Health and Surveillance. 2019;5(4):e14238.
- [CrossRef] [PubMed] [Google Scholar]
- Perceived stress and its associated sociodemographic factors among physicians working in Aseer region of Saudi Arabia. Journal of Liaquat University of Medical and Health Sciences. 2017;16(1):10-8.
- [CrossRef] [Google Scholar]
- Stress, burnout, and strategies for reducing them: what's the situation among Canadian family physicians? Canadian Family Physician. 2008;54(2):234-5.
- [Google Scholar]
- Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Archives of Surgery. . 2009;144(4):371-6.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of stress levels between physicians working in public and private hospitals in Johor, Malaysia. Journal of Taibah University Medical Sciences. 2018;13(5):491-5.
- [CrossRef] [PubMed] [Google Scholar]
- Workplace stress among doctors in government hospitals: an empirical study. International Journal of Multidisciplinary Research. 2012;2(5):208-20.
- [Google Scholar]
- Perceptions of work stress causes and effective interventions in employees working in public, private and non-governmental organisations: a qualitative study. BJPsych Bulletin. 2016;40(6):318-325. DOI: 10.1192/pb.bp.115.050823.
- [CrossRef] [PubMed] [Google Scholar]
- Stress among Doc-tors Doing Residency: A Cross-Sectional Study at a Tertiary Care Hospital in the City of Mumbai. National Journal of Community Medicine. 2015;6(1):21-4.
- [Google Scholar]
- Workload determines workplace Stress among Health Professionals Working in Felege-Hiwot Referral Hospital, Bahir Dar, Northwest Ethiopia. Journal of Environtal & Public Health. 2018;2018 6286010. DOI: 10.1155/2018/6286010.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of the effect of work stress on burnout and quality of life between female nurses and female doctors. Archives of Environmental & Occupational Health. 2011;66(4):193-200.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of shift work on the psychological and physical health of nurses in a general hospital: a comparison between rotating night shifts and day shifts. Risk Manag Healthc Policy. 2016;9:203-211. doi: 10.2147/RMHP.S115326.
- [CrossRef] [PubMed] [Google Scholar]
- Factors affecting working conditions in public hospitals: A literature review. International Journal of Africa Nursing Sciences. 2017;6:28-38.
- [CrossRef] [Google Scholar]
- A literature review of interventions to reduce stress in doctors. Perspectives in Public Health. 2020;40(1):38-53.
- [CrossRef] [PubMed] [Google Scholar]
- Interventions to reduce the consequences of stress in physicians: a review and meta-analysis. J Nerv Ment Dis. 2014;202(5):353-9. doi: 10.1097/NMD. 0000000000000130.
- [CrossRef] [PubMed] [Google Scholar]
- Occupational Stress among doctors-Role of duty schedule and de-stressing techniques. The FASEB Journal. 2020;34(S1):1.
- [CrossRef] [Google Scholar]






