Translate this page into:
Determinants of COVID-19 Vaccine Uptake During Pandemic Times: Insights from Rural Tamil Nadu
*Corresponding author: Geetha Mani, Professor, Department of Community Medicine, Karpaga Vinayaga Institute of Medical Sciences and Research Centre, Chengalpattu, Tamil Nadu, India. drgeethammc@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mani G, Thirumurugan G, Dhandapani T. Learning from the Pandemic: Determinants of COVID-19 vaccine uptake during pandemic times: Insights from rural Tamil Nadu. J Compr Health. 2025;13:72-8. doi: 10.25259/JCH_36_2024
Abstract
Background
COVID-19 vaccines emerged as the mainstay of pandemic control. But the process of vaccinating all the eligible population, unveiled several challenges. With many newer emerging and reemerging diseases necessitating the need for new vaccines, it is essential to recognize the factors which improve vaccine acceptance and uptake among population.
Objectives
To identify the influence of sociodemographic factors and disease- or vaccine-related attitudes on COVID-19 vaccine uptake in rural Tamil Nadu.
Material and Methods
This community-based, study was conducted among 200 randomly selected households from 4 villages of Kancheepuram district, Tamil Nadu, between September and October 2022, using a pretested, semi-structured questionnaire designed to collect information on COVID-19 vaccination status of eligible members of the households and factors associated with vaccine uptake.
Results
91.3% of the eligible population were vaccinated; in 5% households none of the members were vaccinated. Educational status of head of household, comorbidity in family, perceived severity of disease and positive attitude towards vaccine and administrative recommendations were significantly associated with vaccine uptake of households (p≤0.05). Perceived contraindication for vaccine and belief that COVID-19 is a myth were the commonest reasons for non-vaccination.
Conclusion
Attitude towards disease, perceived efficacy of vaccines, along with trust in the administrative recommendations emerged as strong determinants for vaccine acceptance against pandemic circumstances. Vaccination programmes in future should focus on designing appropriate behaviour change communication or advocacy strategies to achieve equitable, universal access to vaccines.
Keywords
COVID-19 vaccine
Determinants
India
Vaccine acceptance
Vaccine uptake
INTRODUCTION WITH OBJECTIVES
Vaccination is enlisted as one of the greatest public health achievements of the 20th century by the Centre for Disease Control.1 In the recent COVID-19 pandemic, vaccines emerged as one of the most essential strategies for pandemic prevention and control.2 To halt the pandemic, there was a need for fair and equitable access to vaccines, starting from the most vulnerable.2 As of 19th April 2024, 85.77% of the Indian population has been fully vaccinated against COVID-19, and 92.57% have received a minimum of one dose.3 Comparing this with the picture on 17th February 2022, a year after the vaccines were introduced, amidst the raging second and third waves of the pandemic, only 55.5% of the Indian population had been completely vaccinated, 69.6% had received one dose, and <1.5% population had received a booster dose.4 With 90.73% and 67.67% of the eligible population partially and fully vaccinated respectively, Tamil Nadu lagged behind few other states.5,6
Estimates till the third quarter of 2021 revealed a marked divide in vaccination rates between urban and rural areas.7 Proportion of adults who were partially immunized and completely immunized was 10–20% lower among suburban and rural areas compared to urban areas.7 The vaccination rates in urban areas were 1.4–1.8 times higher than that of rural areas.7
Among the districts in Tamil Nadu, Kancheepuram district had one of the lowest vaccination rates with 21.33% and 14.88% of the population having received one dose or two doses, respectively, as of 19th February 2022. Thus, it was imperative to identify the possible factors responsible for the above status.8
This picture was a result of the interplay between availability and accessibility factors from the supply side and acceptability factors from the demand side. Awareness, access to vaccines and vaccination centers, transparent information, motivation by employers and community leaders, and lack of better alternatives were found to be enabling factors for COVID-19 vaccine uptake in a multicenter study across India.9 Danabal et al study among rural and urban communities of Tamil Nadu found that older individuals with higher education and occupation had high trust and preferred to get vaccinated.10 Younger age, female gender, rural residence, daily-wage labor, and lower literacy levels were significant factors associated with lower trust and uptake for vaccines.10
Davis et al. in their study in rural areas of six low- and middle-income countries identified common determinants for acceptance or non-acceptance of vaccination. Presumed social norms, positive and negative consequences, anticipated risk and severity of disease, trust, safety, and expected access to COVID-19 vaccines had the highest associations in Bangladesh, Kenya, DRC, and Tanzania. Perceived self-efficacy and trust in information provided by health authorities emerged as possible determinants in Myanmar and India.11
Although we have survived through the worst phases of the COVID-19 pandemic, the emergence and consistent circulation of various strains, recently KP.3, and LB.1, both descendants of JN.1 pose a threat to at-risk and other vulnerable populations. As per the latest COVID-19 epidemiological update released on 15th July 2024, COVID-19 positivity increased from 5.6% to 7.1% in the previous 28-day period. During the same period, new hospitalizations and intensive care admissions also increased by 31% and 12%, respectively.12 For the majority of the world’s population, COVID-19 was the first ever pandemic experienced, and it highlighted the various public health challenges, the most important of them being vaccine hesitancy. Against this scenario, preparedness for a pandemic or any large-scale outbreaks requires countries to actively engage with communities ensuring shared information and active participation. This study might add information about possible community-related factors influencing vaccine acceptance.
While a substantial number of studies had been conducted on the theme during the timeline, the majority of those studies were conducted online due to pandemic restrictions, with an inherent bias of including only those with basic internet literacy and specific educational and occupational groups. The literature review revealed a lack of focused community-level studies addressing the prevalence and determinants of COVID-19 vaccine uptake in rural areas. Hence, this study was planned to assess the proportion of COVID-19 vaccine primary dose uptake in rural areas of the Kancheepuram district and the associated influence of demographic characteristics and attitudes related to disease and vaccines. This was one of the first few studies to be conducted at the community level and hence showcases a balanced view of the vaccination status.
MATERIAL AND METHODS
This was a community-based, cross-sectional study conducted among households of selected villages of the Kancheepuram district of Tamil Nadu between September and October 2022. Households with families having eligible population for COVID-19 vaccination (above 12 years of age) and residing in the area for a minimum of 1 year were included as study population.
Based on the proportion of the population who had received a minimum of one dose of COVID-19 vaccine in the Kancheepuram district (21.33%),8 sample size was calculated using the formula, n = Zα2 pq/d2, where, Za = 1.96, p is the prevalence, q is 100-p and d, an allowable absolute error of 6%. The sample size derived was 179 and considering a possible non-response rate of 10%, the sample size was approximated to 200.
A multistage sampling method was used. Kancheepuram district is divided into 13 Panchayat unions and 648 Village Panchayats. In the first step, 2 Panchayat unions were selected by lottery method. In the second step, two village panchayats were chosen from each of the chosen Panchayat unions by simple random sampling. In the third step, 50 households were selected by systematic random sampling from each of the 4 village panchayats (Arumbuliyur, Kurumanjeri, Manamathy, and Salavakkam) to achieve the required sample size of 200. If any of the chosen households was locked or did not meet inclusion criteria, the next household was contacted. The male or female head of the family was interviewed for relevant details of COVID-19 vaccination status among eligible family members.
A pre-tested, semi-structured questionnaire consisting of the following sections was administered to the participants – basic demographic details of respondents; sociodemographic characteristics of the family including the number of eligible members for vaccination; details of eligible members vaccinated; details of COVID-19 infection in the family; perceived severity of COVID-19 infection; attitude toward COVID vaccination; and reasons for nonvaccination. A 6-item scale with a 5-point Likert response was used to assess attitude toward vaccination with higher scores indicating positive attitude. The attitude scale had a satisfactory Cronbach’s alpha value of 0.861.
Institutional Ethics Committee approval was obtained. Informed written consent was obtained from the participant after explaining the purpose and nature of study. The privacy of the participants and complete confidentiality of information were ensured.
The collected data were entered in Microsoft Excel 2007 and statistical analysis was performed using the Statistical Package for the Social Sciences version 23.0. Categorical variables were expressed as frequencies and percentages and quantitative variables were summarized as mean and standard deviation (SD) or median and inter-quartile range (IQR). The chi-square test or Fisher’s exact test was used for statistical analysis of categorical variables. Quantitative variables were analyzed using the Mann–Whitney U test. A P ≤ 0.05 was considered significant.
Operational definitions
Proportion of COVID-19 vaccine uptake3: Percentage of eligible population from the selected households who have received at least one dose of COVID-19 vaccine
Partially vaccinated3: Individuals who have received a single dose of COVID-19 vaccine
Fully vaccinated3: Individuals who have received both doses of COVID-19 vaccine.
RESULTS
The mean age of respondents was 48.1 years (SD: 11.2). Table 1 describes the baseline characteristics of study population.
| Variable | Frequency (n=200) | Percentage |
|---|---|---|
| Educational status of head of family | ||
| Completed primary | 29 | 14.5 |
| Completed high school | 86 | 43 |
| Higher secondary and above | 85 | 42.5 |
| Type of family | ||
| Nuclear family | 167 | 83.5 |
| Joint family | 33 | 16.5 |
| Frequent travel in family | ||
| Yes | 27 | 13.5 |
| No | 173 | 86.5 |
| Comorbidities in family | ||
| Yes | 60 | 30 |
| No | 140 | 70 |
| Perception of the severity of COVID | ||
| No idea | 32 | 16 |
| Not severe | 1 | 0.5 |
| Somewhat severe | 44 | 22 |
| Severe | 93 | 46.5 |
| Very severe | 30 | 15 |
| Vaccination status of households | ||
| No eligible member in the household vaccinated | 10 | 5 |
| More than 1 eligible member vaccinated | 21 | 10.5 |
| All eligible members vaccinated | 169 | 84.5 |
All the eligible participants in the selected households were assessed for vaccination status.
Among the 200 households, there were 805 persons in the eligible age groups for vaccination, and 735 among them were fully vaccinated (91.3%). The eligible participants were assessed for vaccination status in the following age sub-categories, 12–18 years (202, 25.1%), 18–45 years (316, 39.3%), and above 45 years (287, 35.6%). The maximum proportion of participants was in the 18–45-years age group.
The proportion of the vaccinated population was highest in the 18–45-year age group (296, 93.7%), followed by 12–14 years (187, 92.6%) and above 45 years (252, 87.8%).
All the vaccinated population had received both doses of COVID-19 vaccine. None of the eligible members had received the precautionary or booster dose. Table 2 showcases the distribution of vaccination status based on baseline characteristics.
| Variables | None of the member vaccinated (n=10) | More than 1 member vaccinated (n=190) | Total | Chi-square value |
|---|---|---|---|---|
| Educational status of head of family | ||||
| Completed primary | 5 (17.2) | 24 (82.8) | 29 | 10.82* |
| Completed high school | 3 (3.5) | 83 (96.5) | 86 | P=0.004** |
| Higher secondary and above | 2 (2.4) | 83 (97.6) | 85 | |
| Type of family | ||||
| Nuclear | 8 (4.8) | 159 (95.2) | 167 | P>0.99" |
| Joint | 2 (6.1) | 31 (93.9) | 33 | |
| Frequent travel in family | ||||
| Yes | 1 (3.7) | 26 (96.3) | 27 | P>0.99" |
| No | 9 (5.2) | 164 (94.8) | 173 | |
| Comorbidity in family | ||||
| Yes | 7 (11.7) | 53 (88.3) | 60 | P 0.02'" |
| No | 3 (2.1) | 137 (97.9) | 140 | |
| Perceived severity of COVID-19 infection | ||||
| No idea or not severe | 10 (30.3) | 23 (69.7) | 33 | P<0.000001*" |
| Severe | 0 | 167(100) | 167 | |
Among the 200 households, 21 households (10.5%) reported family history of COVID-19 in the previous 6 months. Out of them, 15 households had eligible members who were nonvaccinated (79.4%). Table 3 shows the distribution of attitude related to vaccine among participants.
| Statements | Distribution of attitude; n (%) | |||||
|---|---|---|---|---|---|---|
| SD | D | N | A | SA | ||
| COVID-19 vaccination is one of the best protective measures against COVID | _ | 2 (1) | 63 (31.5) | 81 (40.5) | 54 (27) | |
| We have a responsibility to be vaccinated to protect others | _ | 9 (4.5) | 73 (36.5) | 73 (36.5) | 45 (22.5) | |
| Vaccinations will help early return to normal outdoor activities and travel | _ | 9 (4.5) | 58 (29) | 87 (43.5) | 46 (23) | |
| We trust in the effectiveness of the COVID vaccine | _ | 4 (2) | 78 (39) | 75 (37.5) | 43 (21.5) | |
| We think vaccination is a way to ensure one’s safety | _ | 2 (1) | 70 (35) | 81 (40.5) | 47 (23.5) | |
| We got vaccinated complying with Health Ministry recommendations | 3(1.5) | 2 (1) | 67 (33.5) | 90 (45) | 38 (19) | |
SD: Strongly disagree, D: Disagree, N: Neutral, A: Agree, SA: Strongly agree
The median attitude score among respondents was 24 with an IQR of 6.75. The households where one or more members were vaccinated (n=190) exhibited a higher median attitude score (Median = 23.26; IQR = 6), compared to households where none of the eligible members were vaccinated (n = 10; Median = 18; IQR = 0). A Mann–Whitney U-test mean rank performed to compare the median attitude scores among the two groups demonstrated a statistically significant difference (P < 0.0001).
Figure 1 highlights the reasons listed by the 31 households where one or more members were not vaccinated. Among the 31 households, perceived contraindication and perception of COVID-19 as a myth were the most common reasons listed by 15 (48.4%) and 10 (32.3%) households, respectively.
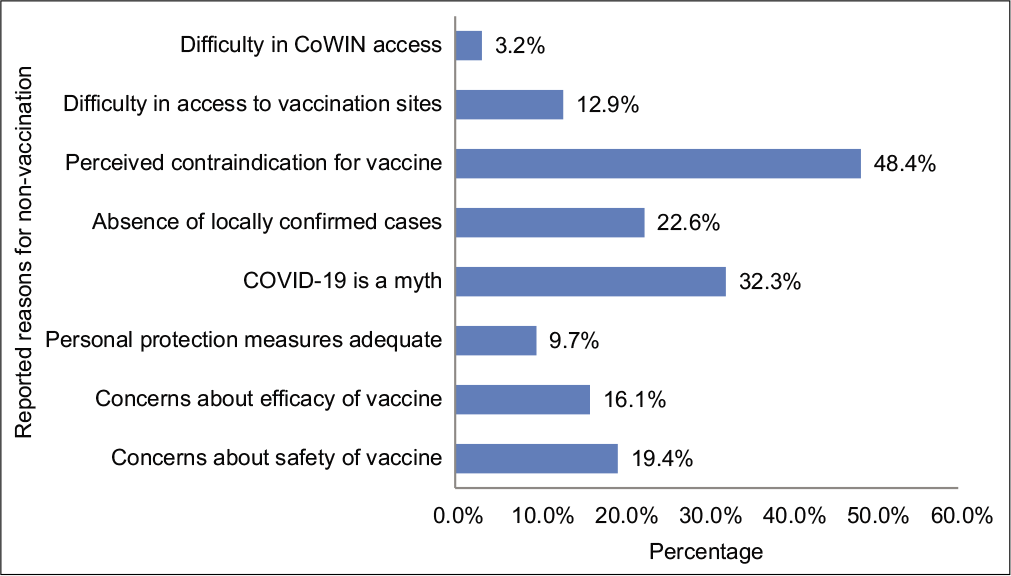
- Distribution of reported reasons for non-vaccination (n = 31).
DISCUSSION
Among the total of 200 study households, 83.5% were living as nuclear families; 13.5% of households reported frequent travel by at least one member, outside the state or country; 60 families (30%) reported chronic comorbid conditions among one or more family members.
An approximate three-fourths of the eligible population belonged to 18–45 years (39.3%) and above 45 years (35.6%). Proportion of vaccination uptake among the eligible population was 91.3% which was higher than the national average during the corresponding period.4-6 An online survey by Kumawat et al. across India reported a higher vaccine acceptance of 97.6%. This margin of difference could be attributed to the possible bias of the more vaccinated population participating in the online survey.13
The lowest proportion was observed in the above 45-year age group (87.8%), despite the fact that people between 45 and 60 years with comorbidity and those above 60 years were the first identified sub-groups of the general population recommended for vaccination. Although the reasons behind individual vaccination status were not explored, the least COVID-19 is a myth uptake among this group could be ascribed to vaccine hesitancy complicated by presumed contraindications, age-induced physical barriers, or inadequate digital literacy preventing access to reliable information and online registration in the CoWIN portal.
In 10 households (5%), none of the eligible members had received vaccine. The educational status of the head of the family and the presence of co-morbid conditions in family members were significantly associated with the vaccination status of families. More than 95% of the households where the head of the family had completed either high school or above have been vaccinated compared to 82.8% of households where the head of the family had less than primary schooling. A similar association between higher educational status and vaccine acceptance was reported by Danabal et al Davis et al Sharma et al, and Senjam et al from studies across India.10,11,14,15 A spatiotemporal exploratory analysis of district-level data on vaccination coverage including all phases of the pandemic by Agarwal and Naha reported a similar positive correlation between literacy rates and vaccination rates.16 Higher educational status may provide access to reliable information on vaccines and required digital literacy for online registration for vaccine appointments. Mandatory registration on the online CoWIN platform for vaccine appointments and the associated language barrier were identified as deterrents to vaccination coverage in early phases by various studies including the current research.
Co-morbidity was acknowledged as a significant positive factor influencing vaccination in the Agarwal and Naha study.16 Our study marginally differed with the findings. The vaccination rates were 88.3% in households with comorbidity compared to 97.9% in households without comorbidity. Despite Government guidelines recognizing those with comorbidity as a priority group, the relatively lesser vaccination rates in households with comorbidity could be due to fear of side effects or the belief of comorbid conditions being a relative or absolute contraindication to vaccination. Co-morbid status being both a positive and negative influence for COVID-19 immunization has been reinforced by a multi-state qualitative study by Godbole et al. where the presence of a health condition was both a motivating and discouraging factor for precautionary dose.17
Respondents from households, who perceived that COVID-19 was severe, had vaccinated more than one member of the family. This finding is similar to the relationship reported by Alqudeimat et al. in Kuwait where perceptions related to the risk of contracting infection and severity of disease were associated with higher vaccination acceptance.18 Perceived severity and vaccination uptake were also reported by Godbole et al.17 in a qualitative study across India and Wong et al. in an online, cross-sectional survey from Hong Kong.19
An approximate 60% had a positive attitude toward various statements on the protective effect of the COVID-19 vaccine and our responsibility to get vaccinated. Danabal et al. reported a positive attitude among more than 50% of the study population in urban and rural areas around Chennai city which was similar to our study findings.10 Although <5% disagreed with any of the statements, the preference for neutrality by close to 30% (29–39%) participants indicates the mixed perceptions and the need to impart adequate authentic information regarding the COVID-19 vaccine and any such program in the future. However, there is a cause for encouragement compared to the Danabal et al study, where a significant proportion showed negative attitudes toward vaccines as well.10 This difference in the attitudes of our study respondents could be explained by the timeline of the studies.
Positive attitude was significantly associated with vaccination status with vaccinated households exhibiting a higher median attitude score (23.26) compared to nonvaccinated households (18). Assuming that the attitude of the respondents reflects the attitude of the family, the difference in median attitude scores could be indicative of the fact that positive attitude has transformed into positive behavior of vaccination of family members. The findings are in concordance with a multinational study including India by Lazarus et al where the positive attitude toward the vaccine was associated with improved acceptance.20 Trust in the safety (odds ratio [OR = 4.46]) and science behind the vaccine (OR = 3.52) and confidence in their Government (OR = 2.13) about equitable and universal access to vaccine were identified as significant attitudes which promote vaccine acceptance. The association was similar among the sub-populations studied in India.20 Perceived self-efficacy and trust in the information provided by the leaders, perceived divine will and perceived action efficacy were identified to be significant determinants of vaccination acceptance in a multicountry study including India by Davis et al in 2021.11 Godbole et al report that trust in the healthcare system, perceived efficacy of vaccine, mandatory vaccination policies were important facilitators for precautionary dose uptake.17
The most commonly reported reason for non-vaccination was the perceived presence of contraindication (48.4%), followed by the assumption that COVID-19 is a myth (32.3%). Concerns about safety (19.4%) or effectiveness (16.1%) of the vaccine and the absence of locally confirmed cases (22.6%) were other reasons reported. This was in concordance with the findings from other studies. Safety and efficacy concerns were reported as important reasons for vaccine hesitancy by Danabal et al and Joshi et al10,21 The reported reasons for non-vaccination and the responses to attitude statements of our participants adhere to the “5C model of drivers of vaccine hesitancy,” confidence, complacency, convenience or constraints, risk calculation, and collective responsibility.22,23 The collective findings related to determinants of vaccine uptake is further strengthened by country-wide qualitative studies by Godbole et al. and Midzi et al. in India and Nigeria, respectively, where geography, safety, and efficacy concerns, various myths and rumors related to vaccine and disease, co-morbidity emerged as important barriers and trust in the health system, availability and accessibility to vaccines, fear of COVID-19, and mortality and mandatory vaccination rules acted as potential facilitators.17,24
Newer outbreaks of Mpox, Chandipura virus encephalitis, Nipah and Zika virus diseases, and other emerging and reemerging infections are testing the capacity and quality of healthcare services in different parts of the world. This study along with other studies highlights the need for timely, transparent information backed by scientific evidence, from Government authorities, made available and accessible to enable people to make informed decisions.
CONCLUSION
This study provides a glimpse of various factors influencing vaccine acceptance against a pandemic. Attitude toward disease, perceived efficacy of vaccines, along with trust in the administrative recommendations emerged as strong determinants. The information obtained will aid in designing appropriate behavior change communication or advocacy strategies to achieve equitable, universal vaccination of eligible populations in future public health emergencies.
Acknowledgment
The authors are grateful to the participants for their whole-hearted participation in the study despite the challenging circumstances caused by the pandemic and associated restrictions.
Ethical approval
The research/study was approved by the Institutional Review Board at Karpaga Vinayaga Institute of Medical Sciences and Research Centre, Chengalpattu District, Tamil Nadu, number KIMS/UG/2022/02, dated 28th August 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Indian Council of Medical Research-Short-term Studentship 2022 (ICMR-STS 2022-Reference ID: 2022-08963).
References
- Ten Great Public Health Achievements-United States, 1900-1999. Morb Mortal Wkly Rep. 1999;48:241-3.
- [Google Scholar]
- Coronavirus Disease (COVID-19): Vaccines. 2022. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-(covid-19)-vaccines?adgroupsurvey={adgroupsurvey}&gclid=eaiaiqobchmi76i1krml9giv2cmrch1nyqp9eaayasaaegl0bpd_bwe [Last accessed on 2022 Feb 15]
- [Google Scholar]
- Vaccinate India Webpage. Available from: https://vaccinateindia.in/dashboard [Last accessed on 2024 Apr 19]
- Our World in Data Coronavirus (COVID-19) Vaccinations. Available from: https://ourworldindata.org/covidvaccinations?country=IND [Last accessed on 2022 Feb 19]
- Cumulative Coverage Report of COVID-19 Vaccination. 2022. Available from: https://www.mohfw.gov.in/pdf/cummulativecovidvaccinationreport15february2022.pdf [Last accessed on 2022 Feb 19]
- [Google Scholar]
- Vaccinate India. Available from: https://vaccinate-india.in/dashboard [Last accessed on 2022 Feb 19]
- [Google Scholar]
- District-wise Estimates of COVID-19 Vaccination Coverage in India. 2021. Available from: https://www.hindustantimes.com/india-news/districtwise-estimates-of-covid-19-vaccination-coverage-in-india-101631036575437.html [Last accessed on 2022 Feb 17]
- [Google Scholar]
- Vaccinate India. Available from: https://vaccinate-india.in/state/31 [Last accessed on 2022 Feb 19]
- [Google Scholar]
- Predictors of COVID-19 Vaccine Confidence: Findings from Slums of Four Major Metro Cities of India. Vaccines (Basel). 2021;10:60.
- [CrossRef] [PubMed] [Google Scholar]
- Attitude Towards COVID 19 Vaccines and Vaccine Hesitancy in Urban and Rural Communities in Tamil Nadu, India-A Community Based Study. BMC Health Serv Res. 2021;21:994.
- [CrossRef] [PubMed] [Google Scholar]
- Behavioural determinants of COVID-19-vaccine acceptance in rural areas of six lower-and middle-income countries. Vaccines (Basel). 2022;10:214.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 Epidemiological Update (169th ed). 2024. Available from: https://www.who.int/publications/m/item/covid-19-epidemiological-update-edition-169 [Last accessed on 2024 Jul 20]
- [Google Scholar]
- Perception, Acceptance, and Adverse Effects of COVID-19 vaccines: Insights from Indian Population. J Family Med Prim Care. 2024;13:1062-7.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 Vaccine Acceptance and its Determinants in the General Population of Delhi, India: A State Level Cross-Sectional Survey. Cureus. 2022;14:e26936.
- [CrossRef] [Google Scholar]
- Vaccination Coverage Against COVID-19 Among Rural Population in Haryana, India: A Cross-Sectional Study. PLoS One. 2024;19:e0299564.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 Vaccine Coverage in India: A District-Level Analysis. Vaccines (Basel). 2023;11:948.
- [CrossRef] [PubMed] [Google Scholar]
- Facilitators and Barriers to the Uptake of COVID-19 Vaccine Precaution Dose Among Adult Population: Qualitative Analysis Across six different States of India. Front Public Health. 2024;11:1293600.
- [CrossRef] [PubMed] [Google Scholar]
- Acceptance of a COVID-19 Vaccine and Its Related Determinants among the General Adult Population in Kuwait. Med Princ Pract. 2021;30:262-71.
- [CrossRef] [PubMed] [Google Scholar]
- Factors Influencing COVID-19 Vaccination Uptake Among Community Members in Hong Kong: A Cross-sectional Online Survey. BMJ Open. 2022;12:e058416.
- [CrossRef] [PubMed] [Google Scholar]
- A Survey of COVID-19 Vaccine Acceptance Across 23 Countries in 2022. Nat Med. 2023;29:366-75.
- [CrossRef] [PubMed] [Google Scholar]
- A Cross Sectional Study to Examine Factors Influencing COVID-19 Vaccine Acceptance, Hesitancy and Refusal in Urban and Rural Settings in Tamil Nadu, India. PLoS One. 2022;17:e0269299.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding COVID-19 Vaccine Hesitancy. Nat Med. 2021;27:1338-9.
- [CrossRef] [PubMed] [Google Scholar]
- Beyond Confidence: Development of a Measure Assessing the 5C Psychological Antecedents of Vaccination. PLoS One. 2018;13:e0208601.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding Facilitators and Barriers to COVID-19 Vaccination in the Zimbabwean Population: A Qualitative Analysis. BMC Public Health. 2024;24:1174.
- [CrossRef] [PubMed] [Google Scholar]







