Translate this page into:
Attitude towards uptake of COVID 19 vaccine among Pregnant Women of Rural and Urban area of North India
CORRESPONDING AUTHOR: Dr Mitasha Singh, Assistant Professor, Department of Community Medicine, ESIC Medical College and Hospital, Faridabad 121001, Haryana E Mail ID: mitasha.17@gmail.com
-
Received: ,
Accepted: ,
CITATION: Aparnavi P, Goswami S, Goyal P, Singh M, Yadav A. Attitude towards uptake of COVID 19 vaccine among Pregnant Women of Rural and Urban area of North India. J Comp Health. 2022;10(2):80-84. Doi: https://doi.org/10.53553/JCH.v10i02.006
Abstract
The objective of the study was to find the uptake of COVID-19 vaccination among pregnant women in an urban and rural area of Faridabad. A cross-sectional study was undertaken in 2021 in a rural and an urban area of Faridabad, chosen by convenient sampling technique. All the antenatal women registered with the accredited social health activists (ASHAs) of the area on the first day of the start of study were included in the study with an exception of those who were not eligible for vaccination as per the Government of India guidelines as of conditions until September 2021. A pre-designed, pre-tested, interviewer-administered questionnaire was used for capturing data. The study recruited 87 pregnant women of which 29 (33.3%) were from urban area and 58 (66.6%) were from rural area. Only 6 (6.9%) of the pregnant women got at least one shot of COVID 19 vaccine. Vaccine uptake in pregnant women was lower than in general population.
Keywords
Immunization
Pregnant Female
Uptake
Sars COVID 19
INTRODUCTION
Non pharmaceutical interventions for coronavirus disease 2019 (COVID-19) like social distancing, face masks, and personal hygiene are currently the mainstay until date. But these are not sustainable methods that can be followed by control of COVID-19 in long term. Hence, herd immunity by vaccination is assumed to be the most effective eradication method, as shown by other viral epidemic diseases in the past. There are evidences showing that transmission of SARS-CoV-2 is lower among people who had vaccination, suggesting that vaccine-acquired herd immunity can be achieved.(1) As per the CDC of the United States, about 25% of the women in reproductive age group (i.e., 15—49 years) who were admitted in hospitals for COVID-19 from March 1st 2020 to August 22nd 2020, were pregnant, and they required mechanical ventilation than nonpregnant women.(2) Pregnant females have a greater risk of severe illness from COVID-19.(3) Their babies also have a higher risk of being born prematurely. Considering the risks of COVID-19 in pregnancy, pregnant women form a priority group to receive the COVID-19 vaccination. The benefits of a vaccine to the people can be achieved not just based on its efficacy, but also on how well it is accepted by the population. Vaccine uptake is at its lowest following the introduction of any new vaccine.(4) As a lower cut off, to achieve herd immunity an estimate of at least 60% to 80% of the people have to be vaccinated.(5) The key factors behind low vaccine uptake include lack of knowledge, fear or lack of trust in the vaccine, not realizing the value of the vaccine, and poor accessibility to the vaccine. Hence this study aims to estimate the prevalence of uptake of COVID-19 vaccination among pregnant women and their perception on vaccine uptake in an urban and rural area of Haryana in North India.
MATERIAL & METHODS
Study design:
A cross-sectional study was conducted in the period between September and December 2021.
Study setting:
It was carried out in the field practice area of tertiary centre of district Faridabad. A rural area (village Pali), and an urban area (Prem Nagar, Sector -7) were chosen by convenient sampling for the area followed by universal sampling of all pregnant women in the area. The population covered under the subcenter Pali was 10,100 and under urban slum area is 3000. There are 400 eligible couples in urban and in rural area.
Sample size:
All the antenatal women registered with the accredited social health activists (ASHAs) of the area were included in the study with an exception of those who were not eligible for vaccination as per the Government of India guidelines as of conditions until September 2021.(6)
Study tool:
A self-designed, pre-tested, interviewer-administered semi-structured questionnaire was used for capturing data on socio-demographic profile, COVID-19 vaccination status in family members, and willingness to get vaccinated.
Ethical Considerations:
Data collection was started after obtaining ethical clearance from the Institutional Ethics Committee (IEC No.134 X/11/13/2021-IEC/41). Written informed consent was received from the participating subjects. At the end of the interview health education was imparted to all the study participants, about the requirement for the vaccine against COVID-19 disease during the ante-natal period and were guided to the nearest vaccination centre or the study site.
Operational Definitions
Registered Pregnant female-A pregnant female irrespective of her gravida and parity who is registered with the ASHA of that area.
Vaccinated with two doses for COVID-19:
Producing the certificate issued by the Government of India, for two doses of any of the COVID-19 vaccines approved by the Government of India as of September 2021.
Partially Vaccinated for COVID-19:
Producing the certificate issued by the Government of India, for one dose of any of the COVID-19 vaccines approved by the Government of India as of September 2021. But not producing a certificate for the second dose.
Covid vaccine uptake:
Getting at least one dose of COVID 19 vaccine was considered vaccine uptake irrespective of their motivation or hesitancy to take the vaccine or the accessibility of the vaccine.
Data collection:
After obtaining the list of all eligible pregnant women from ASHA workers, house to house visit was conducted by the interviewers to reach the pregnant women of that area. Interviewer explained the purpose of study and written consent was obtained.
Data Analysis and Statistical Methods:
Data was fed in the Microsoft excel sheet and cleaned for errors and missing values. The corrected data was analyzed using Epi info version 7 (CDC). The categorical data was given in form of proportions and number.
RESULTS
The study was conducted on a sample of 87 pregnant women of which 29 (33.3%) were from urban area and 58 (66.6%) were from rural area.
Vaccination status:
Only 6 (6.9%) of the pregnant women got at least a single dose of COVID 19 vaccine and all these belonged to rural area. All the eligible family members of 70 (80.4%) of the ante-natal women had got at least a single dose of COVID 19 vaccination. (p<0.01) (Table 1) Significantly, a higher proportion of pregnant women in urban area had all their family members protected with at least one dose of cOvID 19 vaccination. (Table 1)
| Covid 19 vaccine uptake among pregnant women | Rural (n=58) | Urban(n=29) | p value* |
|---|---|---|---|
| Vaccination status | |||
| All the family members of study population vaccinated against COVID-19 | 42 (72.4%) | 28 (96.6%) | <0.01 |
| Received tetanus injection | 55 (94.8%) | 29 (100%) | 0.5 |
| Children fully immunized as per UIP | 58 (100%) | 29 (100%) | - |
| Awareness and perception on COVID 19 vaccination | |||
| Aware about nearest vaccination center | 55 (94.8%) | 15 (51.7%) | <0.01 |
| Aware that pregnant women can be vaccinated according to Government advisory | 18 (31.0%) | 0 (0%) | - |
| Perceive that COVID 19 vaccine is safe | 43 (74.1%) | 18 (62.1%) | 0.3 |
| Perceive that COVID 19 vaccine is safe in pregnancy | 39 (67.2%) | 12 (41.4%) | 0.03 |
*Chi square/ Fischer test
All the pregnant women in urban area had received at least one dose of tetanus toxoid (Td) during the current pregnancy but 3(5.6%) of those in rural area did not receive even one dose.
Awareness:
Majority; (79.3%, 69/87) were not aware that COVID19 vaccines were advised by the government for pregnant women also and (6/18) 33% of women who were aware took the vaccine. (Table 2) Among those who were aware that they can be vaccinated, 11.1% (2/18) did not receive vaccination because it was not available and one person from rural area could not receive because of technical issues (UID/Aadhaar card issues). Majority; (79%, 64/81) of the unvaccinated were aware about the nearest vaccination center in their area. (Table 2) Significantly, a higher proportion of the rural women were aware of the nearest vaccination center. (Table 2)
| Covid 19 vaccine uptake among pregnant women | Vaccinated (n= 6, 10.3%) | Unvaccinated (n=52, 89.6%) | p value* |
|---|---|---|---|
| Vaccination status | |||
| All the family members of study population vaccinated against CoViD-19 | 2 (33.3%) | 40 (76.9%) | 0.04 |
| Received tetanus injection | 6 (100%) | 49 (94.2%) | 1 |
| Children fully immunized as per UIP | 6 (100%) | 52 (100%) | - |
| Awareness and perception on COVID 19 vaccination | |||
| Aware about nearest vaccination centre | 6 (100%) | 49 (94.2%) | 1 |
| Aware that pregnant women can be vaccinated according to Government advisory | 6 (100%) | 12 (23.1%) | <0.01 |
| Perceive that COVID 19 vaccine is safe | 6 (100%) | 37 (71.1%) | 0.3 |
| Perceive that COVID 19 vaccine is safe in pregnancy | 5 (83.3%) | 34 (65.3%) | 0.6 |
*Chi square/ Fischer test
Perception:
Only 4 (4.6%) believed that covid during pregnancy can have serious consequences like abortion, death of the child and all the others reported that they do not know about the consequences of covid in pregnancy. All those who were aware of consequences of Covid 19 were vaccinated against it. Majority of pregnant females 65 (74.7%) felt vaccine might protect against COVID-19 disease. Majority of the unvaccinated (67.9%, 55/81) believed the vaccine was safe for general population. (Table 2) One woman who received the vaccine said she did not know if it was safe but took it because her ASHA worker advised her to. Significantly, higher proportion of women in rural area perceived that COVID 19 vaccination is safe in pregnancy.
For pregnant women:
Of the 81 unvaccinated pregnant women, majority 38 (46.9%) said that will get vaccinated after delivery, but 31(38.3%) said that they are not willing to get vaccinated even after delivery and 12 (14.8%) were willing to get vaccinated now. (Figure 1)
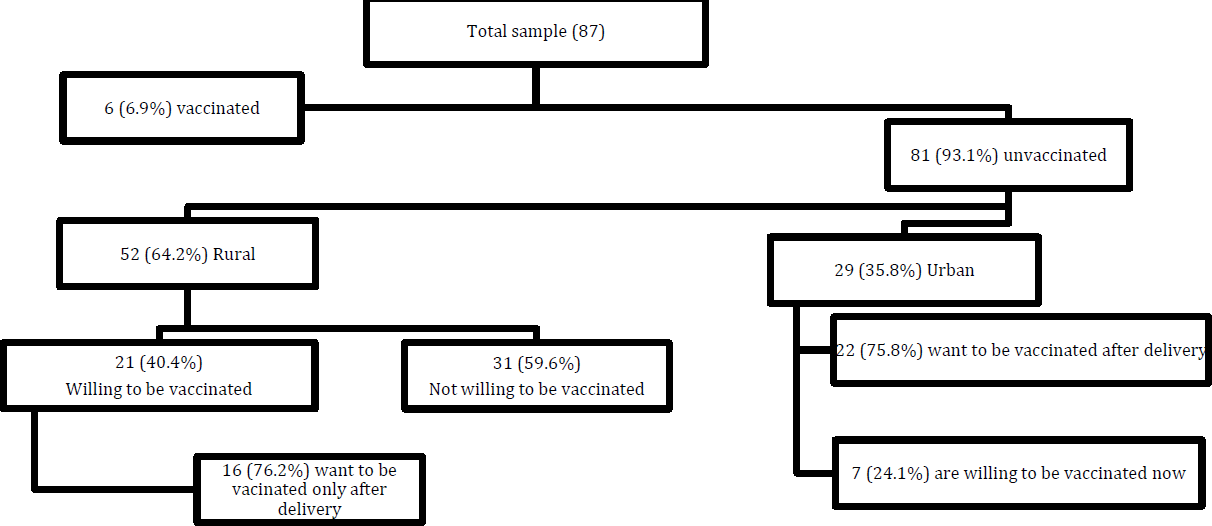
- WILLINGNESS TO ACCEPT COVID 19 VACCINATION AMONG PREGNANT WOMEN
Influencer for vaccine uptake:
Only 43 respondents answered this question. All the 12(14.8%) who were willing to be vaccinated if their ASHA/ AWW worker advices for it. Majority (76.3%, 29/38) of those who wanted to delay vaccination until delivery also said that they would take the vaccination if ASHA/ AWW worker advices for it. Similarly, the 69 who were not aware if they can be vaccinated during pregnancy relied on their ASHA/ANM for update on vaccination for pregnant women.
DISCUSSION
This study intended to examine, the uptake of COVID-19 vaccines by antenatal women in Faridabad, Haryana. The study was done on pregnant women of both rural and urban area. Reports across the globe showed a higher acceptance and willingness for the vaccine against COVID-19 disease (7,7) but in the current study among pregnant women willingness was present but delayed it until delivery. In accordance, a study conducted in 2022 (9) also reported that COVID 19 vaccine acceptance was lower in pregnant females than the general population. In India also nearly half the eligible general population had taken a minimum of single dose of vaccine but among pregnant women in our study the uptake was much lesser. The vaccinated study population belonged to rural area. Owing to a small number findings cannot be generalized. However, it points towards reduction in urban rural disparity in terms of primary health services through field workers.
Previous studies during the pandemic situation had showed that people trusted their personal physicians to be their reliable person for vaccine related knowledge.(10) Current study revealed the reliance and faith on community health workers’ (ASHA/AWW) advise by the ante natal women. This might be because the participants were registered with the ASHA worker of the area and hence are those tracked and motivated by health care workers. A study on pregnant women of Turkey (11) have also considered tetanus vaccine uptake and awareness about its importance as a proxy for increasing uptake of Covid vaccine during pandemic. This could have been a motivating factor for higher proportion of pregnant female in making their COVID 19 vaccination decision based on ASHA/ AWW workers advice. Around 62% of non-vaccinated antenatal women were ready to take the Covid vaccine in near future. This was higher in comparison to the studies on pregnant women in Turkey (11) where 37% wanted to get vaccinated and the study in France (12) where 29.5% wanted to get vaccinated. Even though the period of data collection was in concordance with the current study, the study done in 16 countries (13) 52% intended to get COVID 19 vaccine in the ante-natal period with India being one among the highest acceptors.
Since, it was revealed that high proportion of participants based their decision on field workers, we also had a discussion with the ASHA and Anganwadi workers regarding the same. It was understood that many of them did not specifically receive official communication to vaccinate pregnant women. Thus, indicating a delay in communication from the health care system. Safety concerns about vaccine was another common reason for reduced uptake of Covid vaccine. Similar findings were reported by Ayhan GS, et al.,(11) from Turkey and Egloff C, et al.,(12) from France. One of the limitations of the study was that it was conducted one month after release of guidelines for pregnant women hence the implementation delay could be attributed to the early conduction of evaluation survey.
CONCLUSION
The study concludes that COVID 19 vaccine uptake rate for ante-natal women was low even though majority of them had all their eligible family members vaccinated. The opportunity of primary health care providers working in the environment of the beneficiaries must be utilised at the frontline in the efforts to tackle COVID-19 vaccine hesitancy and in behavioural change communication.
To assist ante-natal women decide on vaccination, they must receive information about the effects of COVID-19 disease during pregnancy and the likely benefits of receiving vaccination in the local epidemiological context. They should also be made aware about the current limitations of safety records among ante-natal people.
REFERENCES
- WHO Coronavirus (COVID-19) Dashboard | WHO Coronavirus (COVID-19) Dashboard With Vaccination Data (no date) Available at: https://covid19.who.int/ (accessed )
- [Google Scholar]
- BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting. The New England journal of medicine. 2021;384(15):1412-1423.
- [CrossRef] [PubMed] [Google Scholar]
- Morbidity and Mortality Weekly Report Characteristics and Maternal and Birth Outcomes of Hospitalized Pregnant Women with Laboratory-Confirmed COVID-19-COVID-NET, 13 States. 2020
- [Google Scholar]
- The Moderna COVID-19 (mRNA-1273) vaccine: what you need to know (no date) Available at: https://www.who.int/news-room/feature-stories/detail/the-moderna-covid-19-mrna-1273-vaccine-what-you-need-to-know (accessed )
- [Google Scholar]
- anne. Understanding vaccine hesitancy in COVID-19. Med (New York, N.y.) . 2021;2(5):498.
- [CrossRef] [PubMed] [Google Scholar]
- Safety Concerns Remain Main Driver of Vaccine Hesitancy -AP-NORC (no date) Available at: https://apnorc.org/projects/safety-concerns-remain-main-driver-of-vaccine-hesitancy/ (accessed )
- [Google Scholar]
- Looking beyond COVID-19 vaccine phase 3 trials. Nature medicine. 2021;27(2):205-211.
- [CrossRef] [PubMed] [Google Scholar]
- A global survey of potential acceptance of a COVID-19 vaccine', Nature Medicine. . 2021;27(2):225.
- [CrossRef] [PubMed] [Google Scholar]
- Women's views on accepting COVID-19 vaccination during and after pregnancy, and for their babies: a multi-methods study in the UK. 2022. BMC Pregnancy and Childbirth. 22:1-15.
- [CrossRef] [PubMed] [Google Scholar]
- KFF COVID-19 Vaccine Monitor: January 2021 -Vaccine Hesitancy -9616-2 | KFF (no date) Available at: https://www.kff.org/report-section/kff-covid-19-vaccine-monitor-january-2021-vaccine-hesitancy/ (accessed )
- [Google Scholar]
- COVID-19 vaccine acceptance in pregnant women', International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. . 2021;154(2):291-296.
- [CrossRef] [PubMed] [Google Scholar]
- Pregnant women's perceptions of the COVID-19 vaccine: A French survey. PloS one. 2022;17(2):e0263512.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 vaccine acceptance among pregnant women and mothers of young children: results of a survey in 16 countries', European journal of epidemiology. . 2021;36(2):197-211.
- [CrossRef] [PubMed] [Google Scholar]






