Translate this page into:
Body Mass Index as an Indicator of Psychological Well-being and Memory Functioning in Middle-aged Indian Adults
*Corresponding author: Susmita Halder, Department of Psychology, St. Xavier’s University, Kolkata, West Bengal, India. susmitahalder@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Halder S, Chakravarty S. Body Mass Index as an Indicator of Psychological Well-being and Memory Functioning in Middle-aged Indian Adults. J Compr Health. 2025;13:65-71. doi: 10.25259/JCH_39_2024
Abstract
Background
Body mass index (BMI) has long been an important parameter of concerns ranging from hypertension to hyperglycemia. Alongside these medical conditions, BMI is seen to be equally effective in predicting psychological correlates including well-being and cognition focusing on memory functioning.
Objectives
The objectives of the study are to study the sub-domains of memory and perception of psychological well-being (PWB) in high and normal BMI groups comprising middle-aged adults.
Material and Methods
A cross-sectional study was conducted on an urban population comprising adults in the age range of 40–60 years. Data were obtained from more than 60 individuals who were further screened to be grouped into two categories, namely one with a BMI value normal: 18.5–24.9 and another with a BMI measure equal to and above 25 (obese), each comprising data of 30 distinct individuals. A questionnaire survey followed by a psychometric test was administered to the participants.
Results
Findings suggest a significant correlation of 0.427 between normal BMI and memory functioning, PWB and memory functioning, and also significant mean differences between aspects of PWB, like autonomy, and personal growth, and sub-domains of memory functioning like a recent memory, remote memory, and mental balance across the two groups.
Conclusion
The present study has indicated that BMI is an indicator in determining memory functioning and well-being in middle-aged adults in an urban population.
Keywords
Body mass index
Memory functioning
Metabolic syndrome
Psychological well-being
INTRODUCTION WITH OBJECTIVES
Health serves as the sole basis for striking that even balance between life and its crippling odds. As understood commonly, health implies a state of wellness in connection with a condition indicating the absence of disease or injury. Health and sickness are not entirely separate concepts - they overlap.1 The premise broadened to include the perception of physical, mental, and social well-being. Health, as understood commonly, refers to a state where an active individual may not only be free of injury, or illness but also experience an even balance between one’s physical and psychological well-being (PWB).
The different biological processes taking place within the human body are inextricably enmeshed in the specific structural labyrinths. In a way, metabolism is referred to the different chemical reactions taking place within living beings. It may be broadly classified into anabolism and catabolism. Anabolic is responsible for the growth and addition of complex substances from relatively fundamental units. On the other hand, catabolism refers to the process of breakdown of complex, larger structures into simpler units utilized by the cells of the body. It may be said that anabolic and catabolic processes collectively make up a well-integrated system of bodily processes. The simplest expression of body mass index (BMI) is body weight (in kg) and the squared value of height (in m2). BMI serves as an indicator of body fatness, leading to classifying and categorizing individuals into groups. Since ages, body fatness has manifested a prominent stature in psychosocial narratives of desirability, and acceptance of oneself, both at personal and societal levels [Figure 1].2
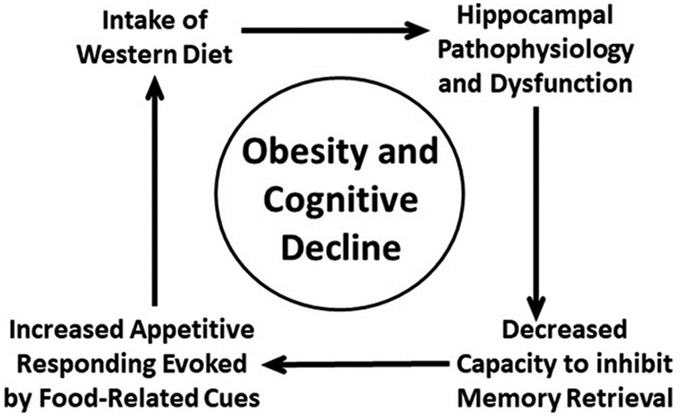
- Connection between obesity and cognitive decline.
In this context, metabolic syndrome3 is a condition that is principally indicated by the measure of BMI, highlighting the premise of physical health entailed by body weight against individuals’ height, facilitating its determination. This condition refers to a cluster of pathological conditions that heighten the risk of suffering from coronary heart disease, diabetes mellitus, myocardial infarction, and other serious health problems. This condition is featured by a large waistline, hypertension, increased concentration of triglycerides, and lessening of high-density lipoprotein HDL (good) cholesterol. PWB is one of the three distinct well-being concepts.4 It encompasses different perspectives on life. These essentially lie beyond the scope of health, further into the domains of self-esteem, efficacy, interpersonal relations with others, and a feeling of satisfaction. Nonetheless, from a monastic perspective, it may be said that both physical and PWB are strongly interrelated. Memory functioning may be seen as a global function encompassing a wide range of other cognitive functions as mentioned. The assessment of memory, in the context, was focused on the functional aspects of “memory” including remote memory, recent memory, mental balance, attention and concentration, delayed and immediate recall, and verbal retention of similar and dissimilar pairs. Studies suggest that BMI within the normal range indicates a likelihood of greater PWB and significantly higher memory functioning5 whereas a negative correlation exists between high BMI and PWB.6,7 The present study was conducted in a population of age ranging between 40 and 60 years. This typically qualified for a middle-aged population. This age group marks a transitory phase between an adventurous, thrill-seeking young adulthood and a retired life, accompanied by a sense of fulfillment of duties and responsibilities, contentment from successfully achieving one’s life goals, and gratitude for the divineness of life and its splendor. The various changes that set in are carefully looked into, as those serve as important markers in determining the changed life-path trajectory of individuals.8
The present study is aimed at investigating the existence of any potential relationship between BMI measure and PWB and memory functioning of middle-aged adults.
MATERIAL AND METHODS
This is a correlational cross-sectional study. The study sample comprised 60 individuals belonging to urban and suburban communities, located in and around Kolkata. Screening was done based on the inclusion and exclusion criteria stated ahead. Data were collected over a period of 4 months, ranging from January to April 2023. This sample was further classified into two groups based on the BMI measure, namely high BMI (BMI ≥24.9) and normal BMI (BMI: 18.5–24.9), each group having 30 individuals from a sample of 60 individuals. The sample was constructed using a purposive sampling technique. The study included individuals, both males and females, in the age range of 40–60 years, having basic educational qualifications and can read, write, and comprehend simple instructions, and particularly excluded individuals who presented with significant physical, psychological, or neurological illness. Informed consent was taken from each participant and ethical standards were maintained.
Tools used in the present study are as follows:
Sociodemographic details and clinical datasheet: This consists of the preliminary information of the concerned individual, including name, age, sex, education, occupation, socioeconomic status, residence, and family type. Such personal details were obtained exclusively to investigate the difference between the respective sociodemographic variables determining an individual’s likely performance. No significant personal information was revealed hence anonymity was maintained throughout.
Height and weight measuring scales: The height and weight measures of each individual were measured using a standard weighing machine and inch-wise calibrated measuring tape.
Ryff ’s PWB scales (RPWBS): Developed by psychologist Carol D. Ryff, the 42-item PWB scale measures 6 aspects of well-being and happiness: Autonomy, environmental mastery, personal growth, positive relations with others, purpose in life, and self-acceptance.3 Researchers have used both the 42-item PWB scale and a shortened 18-item version.9,10 The current study has been conducted using the shortened 18-item version. RPWBS’s test-retest reliability was found to be 0.82.11
Postgraduate institute battery of brain dysfunctions: This instrument was aimed to assess the overall memory functioning of middle-aged individuals, located in different urban communities of Kolkata.12 This tool measures a multitude of cognitive processes related to memory and quantifies cognitive dysfunction, impairments, and significant declines and deficits in clinical settings. For the current study, out of the many assessment scales that this battery contains, the Post-Graduate Institute (PGI) memory scale has been used to assess the memory functioning of middle-aged adults. The different sub-domains assessed are remote memory, recent memory, mental balance, attention and concentration, delayed recall, immediate recall, verbal retention of similar pairs, and verbal retention of dissimilar pairs.
The study aims to analyze the relationship between PWB, memory functioning, and BMI values using correlation analysis. Specifically, the correlation coefficient between PWB and normal BMI values will be examined to determine the presence and direction of association. Similarly, the correlation between PWB and high BMI values will be assessed to identify potential trends. In addition, the study will investigate the correlation between memory functioning and normal BMI values to evaluate the significance and strength of their relationship. Finally, the correlation between memory functioning and high BMI values will be analyzed to explore potential negative associations. The statistical significance of these correlations will be determined based on the given P-value criteria.
RESULTS
The study at hand aims to determine the relationship between BMI and PWB and memory functioning in middle-aged adults. This study was conducted on middle-aged adults, residing in different communities, located in and around Kolkata. The age of individuals lying in this population typically ranges between 40 and 60 years and the sample comprised a total of 60 individuals with 30 individuals lying in the normal BMI range, i.e., 18.5–24.9, and the rest 30 individuals lying in the BMI range in and above 25. The results are depicted in tables in the following section.
DISCUSSION
In Table 1, the other important sociodemographic variables, namely gender, marital status, occupation, family type, religion, and residence, are analyzed across two groups using descriptive statistics such as frequency and percentage. In Group-A, i.e., individuals having BMI within range, 16 (53.3%) males and 14 (46.7%) females are present; 30 (100%) individuals are married; 17 (56.7%) of them are into service, 3 (10%) of them are into business, 9 (30%) individuals are unemployed, and 1 (3.3%) of them is self-employed; 11 (36.7%) individuals belong to joint family, whereas 19 (63.3%) belong to nuclear family; 29 (96.7%) individuals practice Hinduism, and 1 (3.3%) practices Buddhism; and, 27 (90%) of them live in urban setting, and the rest 3 (10%) reside in suburban setting. In Group-B, 16 (53.3%) males and 14 (46.7%) females are present; 29 (96.7%) individuals are married and 1 (3.3%) is unmarried; 18 (60%) of them are into service, 3 (10%) of them are into business, 7 (23.4%) individuals are unemployed, 1 (3.3%) of them is self-employed, and 1 (3.3%) is a retired professional; 12 (40%) individuals belong to joint family, whereas 18 (60%) belong to a nuclear family; 29 (96.7%) individuals practice Hinduism, and 1 (3.3%) practices Christianity; and, 26 (86.7%) of them live in an urban setting, and the rest 4 (13.3%) reside in suburban setting.
| Variable | Sub-domain | Normal BMI | High BMI | ||
|---|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | ||
| Gender | Male | 16 | 53.3 | 16 | 53.3 |
| Female | 14 | 46.7 | 14 | 46.7 | |
| Marital status | Married | 30 | 100 | 29 | 96.7 |
| Unmarried | 0 | 0 | 1 | 3.3 | |
| Occupation | Service | 17 | 56.7 | 18 | 60 |
| Business | 3 | 10 | 3 | 10 | |
| Self-employed | 1 | 3.3 | 1 | 3.3 | |
| Retired | 0 | 0 | 1 | 3.3 | |
| Unemployed | 9 | 30 | 7 | 23.4 | |
| Family type | Joint | 11 | 36.7 | 12 | 40 |
| Nuclear | 19 | 63.3 | 18 | 60 | |
| Religion | Hinduism | 29 | 96.7 | 29 | 96.7 |
| Buddhism | 1 | 3.3 | 0 | 0 | |
| Christianity | 0 | 0 | 1 | 3.3 | |
| Residence | Urban | 27 | 90 | 26 | 86.7 |
| Suburban | 3 | 10 | 4 | 13.3 | |
BMI: Body mass index
In the above Table 2a, one of two variables of this study, PWB is carefully analyzed across the two groups of individuals with normal and high BMI, respectively. In the difference of means of respective sub-domains between the two groups, means and standard deviation values have been analyzed and interpreted. The t-value indicates the difference between means. The first of the six sub-domains, autonomy, has a t-value of 1.184 at a P-value of 0.375, thus suggesting the difference between means to be not significant. The second in line is environmental mastery having a t-value of 0.177 at a P-value of 0.337, where the difference is not significant. The third sub-domain, personal growth has a t-value of 1.768 at a P-value of 0.317, suggesting the value to be insignificant. Followed by positive relations with others, where the t-value is 0.586 at a P-value of 0.594, suggesting the difference between means to be insignificant. The fifth sub-domain, purpose in life, has a t-value of 0.617 at a P-value of 0.548, where the value is insignificant. The last sub-domain, self-acceptance has a t-value of 0.581 at a P-value of 0.147, at which the difference between the means of the two groups is insignificant.
| Variables | Sub-domains | Normal BMI | High BMI | t-value | P-value | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Psychological well-being | Autonomy | 15.4 | 4.039 | 14.23 | 3.579 | 1.184 | 0.375 |
| Environmental mastery | 16.6 | 3.114 | 16.47 | 2.713 | 0.177 | 0.337 | |
| Personal growth | 19 | 2.228 | 17.87 | 2.713 | 1.768 | 0.317 | |
| Positive relations with others | 16.2 | 3.773 | 16.77 | 3.711 | 0.586 | 0.594 | |
| Purpose in life | 15.03 | 3.057 | 15.57 | 3.617 | 0.617 | 0.548 | |
| Self-acceptance | 16.27 | 3.29 | 16.73 | 2.924 | 0.581 | 0.147 | |
BMI: Body mass index, SD: Standard deviation
In Table 2b, obtained data on memory functioning were statistically treated across the two groups of individuals with normal and high BMI, respectively. The difference between means of respective sub-domains between the two groups, mean, and standard deviation values for each sub-domain have been analyzed and interpreted. The t-value indicates the difference between means. The first of the six sub-domains, remote memory, has a t-value of 1.512 at a P-value of 0.003, thus suggesting the difference between means is significant at this P-level. The second in line is recent memory having a t-value of 1.000 at a P-value of 0.043, where the difference between means is significant at the given P-level. The third sub-domain, mental balance has a t-value of 1.143 at a P-value of 0.022, suggesting the difference to be significant at the P-value. Followed by attention and concentration, where the t-value is 0.569 at a P-value of 0.157, suggesting the difference between means to be insignificant. The fifth sub-domain, delayed recall, has a t-value of 0.977 at a P-value of 0.392, where the value is insignificant. The following subdomain, immediate recall, has a t-value of 0.738 at a P-value of 0.506, at which the difference between the means of the two groups is insignificant. In the next sub-domain in line, verbal retention of similar pairs has a t-value of 0.684 at a P-value of 0.172, where the value stands insignificant. The last sub-domain, verbal retention of dissimilar pairs has a t-value of 0.646 at a P-value of 0.953, where the difference between means across the two groups is not significant.
| Variables | Sub-domains | Normal BMI | High BMI | t-value | P-value | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Memory functioning | Remote memory | 5.9 | 0.305 | 5.73 | 0.521 | 1.512 | 0.003 |
| Recent memory | 4.97 | 0.183 | 5 | 0.03 | 1 | 0.043 | |
| Mental balance | 8.07 | 1.258 | 7.67 | 1.446 | 1.143 | 0.022 | |
| Attention and concentration | 11.33 | 2.264 | 11.03 | 1.79 | 0.569 | 0.157 | |
| Delayed recall | 8.97 | 1.402 | 9.3 | 1.236 | 0.977 | 0.392 | |
| Immediate recall | 9.17 | 1.84 | 8.8 | 2.007 | 0.738 | 0.506 | |
| Verbal retention of similar pairs | 4.8 | 0.407 | 4.87 | 0.346 | 0.684 | 0.172 | |
| Verbal retention of dissimilar pairs | 8 | 4.283 | 8.7 | 4.103 | 0.646 | 0.953 | |
BMI: Body mass index, SD: Standard deviation, Bold denotes significance values given as P-value.
Table 3 explains the relation between variables. The relation has been obtained by computing Pearson’s correlation coefficients between the desired variables. The correlation coefficient obtained between PWB and normal BMI values is 0.217 at a P-value of 0.248, suggesting a positive correlation though not significant. The correlation coefficient between PWB and high BMI values is −0.002 at a P-value of 0.993, suggesting a negative correlation between the two, however, not significant. The correlation coefficient between memory functioning and normal BMI value is 0.427 at a P-value of 0.018 suggesting a significant positive correlation between the two. Finally, the correlation coefficient between memory functioning and high BMI value is −0.282 at a P-value of 0.131 suggesting a negative correlation between the two that is not significant at the given P-value.
| Group | Psychological well-being | Memory functioning | ||
|---|---|---|---|---|
| Pearson's correlation coefficient (r) | P-value | Pearson's correlation coefficient (r) | P-value | |
| Normal BMI | 0.217 | 0.248 | 0.427 | 0.018 |
| High BMI | -0.002 | 0.993 | -0.282 | 0.131 |
BMI: Body mass index
The current study aimed to investigate the relationship between the physiological measure of BMI and affective and cognitive domains of PWB and memory functioning, respectively, in middle-aged adults, based in and around Kolkata.
As studies indicate, BMI is an integral parameter in determining metabolic syndrome, a condition that heightens the risk of atherosclerotic cardiovascular disease, diabetes mellitus, insulin resistance, and vascular and neurological conditions. A normal BMI ranging between 19 and 24.5 can reduce the likelihood of developing metabolic syndrome among adults. The study at hand draws a comparison between two groups, namely individuals with a BMI of 25 and value of 25 and below, i.e., normal BMI (Group-A), and individuals having a BMI of 25 and above, i.e., high BMI (Group-B), based on PWB and memory functioning. The mean BMI for groups A and B was found to be 23.58 and 28.53, respectively. As some studies suggest that a BMI of 27 is optimum to identify metabolic syndrome in men and women,13 it may be stated that for Group B, the mean BMI indicates a potential condition for the development of metabolic syndrome in such individuals.
The existing body of research literature has held a considerably consistent position inferring that higher BMI value is associated with lower well-being (including Subjective, Emotional, and PWB), in studies emphasizing BMI-related variables such as obesity, weight loss, and the like.14,15
In the present study, findings drawn on PWB across the two groups reveal that BMI values do not have a considerably significant impact on the PWB of individuals with either high or low BMI. Here, it may be stated that the majority of these studies were based in developed countries where physical health and wellness are major social concerns that are effectively addressed by individuals, subsequently, it is reflected in their PWB measure, in contrast to individuals living in developing countries like India.16 Here, the majority of individuals are not well-informed about physical health measures like BMI, and its relation with metabolic and visceral processes of the body, as well as individual’s psychological health resulting in an even assessment of PWB. As a result, across a wide range of BMI values, no significant impact is evident on an individual’s self-reported responses to PWB measures.
The relationship between BMI and PWB, and memory functioning, respectively, indicates that there is a positive relationship between normal BMI and PWB and memory functioning, suggesting that with BMI within the normal range, there is a greater likelihood of positive PWB and a significantly higher memory functioning, whereas, a negative correlation exists between high BMI and PWB6 and memory functioning,5 suggesting that higher the BMI value lower PWB of individual and reduced memory functioning.7
Results drawn on memory functioning across the two groups imply that there exist significant differences in sub-domains determining memory functioning, in middle-aged adults. Existing research findings suggest that memory functioning is most affected in individuals suffering from metabolic syndrome. Studies suggest that metabolic conditions, namely hyperglycemia, hyperinsulinemia, biogenic dysfunction, and inflammation, have a debilitating impact on the hippocampus circuit that is instrumental in memory functioning.17,18 The presence of metabolic disorders leads to cognitive decline in individuals.19 Results drawn on memory functioning across the two groups imply that there exist significant differences in sub-domains determining memory functioning, in middle-aged adults. Studies linking obesity and memory deficits in young and middle-aged adults20 suggest that obesity (high BMI condition) is related to reduced memory performance in older adults. In the present study, it was found that in the specific sub-domains of memory, namely remote memory, recent memory, and mental balance, significant differences exist between the means of the two groups owing to their P-values. On the other hand, it was found that in the specific sub-domains of memory, namely remote memory, recent memory, and mental balance, significant differences exist between the means of the two groups owing to their P-values. Here, it may be said that PWB is rated by the individual on being administered a self-report inventory, where the individual’s subjective responses have been recorded. Performance on memory tasks was evaluated by administering a test having room for objective assessment. Thus, it reflects that an individual’s perception of well-being may not be affected by their physical health conditions owing to a lack of awareness of health specifics, however, memory being a function of cognitive and neuro-psychological domains indicates a connection between physical health measures and the state of psychological wellness.
The present study specifically dealt with two psychological aspects, namely the affective component; PWB, and the cognitive component; memory functioning, against a physical measure of BMI, and the findings of this study will cater to the majority of the masses belonging to middle socioeconomic status, who had basic to advance educational qualification, thus constituting the active working population of the society. However, since the sample size was small owing to the procedure being a non-probability sampling technique, the findings from the study may be a reflection of the urban and suburban population in localities present in and around Kolkata, yet findings may not be generalized owing to a non-probability sampling technique being used to constitute the sample. The study has not just limited its extent to BMI determination and associated effects but has also concluded its explanations on aspects like metabolic syndrome, and its timely detection in its tenets of discussion that may serve to be beneficial for readers, who in turn, may foster an awareness among the masses, and further future research in this domain and its allied streams.
CONCLUSION
The findings of this study highlight that BMI serves as a significant indicator of PWB and memory functioning in middle-aged Indian adults. A positive relationship was observed between normal BMI and both PWB and memory functioning, indicating that maintaining a BMI within the normal range is associated with greater psychological resilience and enhanced cognitive performance. Conversely, a negative correlation was identified between high BMI and these parameters, suggesting that an elevated BMI is linked to reduced PWB and impaired memory functioning. These results underscore the importance of promoting healthy weight management strategies to enhance both mental and cognitive health in middle-aged populations.
Ethical approval
Institutional Review Board approval is not required since the present study was a part of dissertation certified by the mentioned affiliation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Health Psychology: Biopsychosocial Interactions United States: John Wiley and Sons; 2014.
- [Google Scholar]
- The Cognitive Control of Eating and Body Weight: It's More than What You “Think”. Front Psychol. 2019b;10:62.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and Management of the Metabolic Syndrome. Circulation. 2005;112:2735-52.
- [CrossRef] [PubMed] [Google Scholar]
- Eudaimonic Well-being: Highlights from 25 Years of Inquiry In: Diversity in Harmony-insights from Psychology: Proceedings of the 31st International Congress of Psychology. Chichester, UK: John Wiley and Sons Ltd.; 2018. p. :375-95.
- [CrossRef] [Google Scholar]
- Obesity and Neurocognitive Performance of Memory, Attention, and Executive Function. NeuroSci. 2022;3:376-86.
- [CrossRef] [PubMed] [Google Scholar]
- The Impact of Obesity on Psychological Well-being. Best Pract Res Clin Endocrinol Metab. 2005;19:421-40.
- [CrossRef] [PubMed] [Google Scholar]
- Obesity and Impaired Cognitive Functioning in the Elderly: A Population-based Cross-sectional Study (NEDICES) Eur J Neurol. 2013;20:899-906, e76-7
- [CrossRef] [PubMed] [Google Scholar]
- The Structure of Psychological Well-being Revisited. J Pers Soc Psychol. 1995;69:719-27.
- [CrossRef] [PubMed] [Google Scholar]
- Subjective and Objective Hierarchies and their Relations to Psychological Well-being: A US/Japan Comparison. Soc Psychol Personal Sci. 2014;5:855-64.
- [CrossRef] [PubMed] [Google Scholar]
- The Relationship of Psychological Well-being With Marital Quality and the Dimensions of the Married Students. Indian J Sci Res. 2014;7:534-8.
- [Google Scholar]
- 1990. Handbook of PGI Battery of Brain Dysfunction (PGI-BDD) ScienceOpen. Available from: https://www.scienceopen.com/document?vid=c6678cf1-805f-4016-b8db-dc3a75792bb2 [Last accessed on 2024 Sep 07]
- Normal Body Mass Index (BMI) Can Rule Out Metabolic Syndrome. Medicine (Baltimore). 2019;98:e14712.
- [CrossRef] [PubMed] [Google Scholar]
- Obesity and Physical and Emotional Well-being: Associations between Body Mass Index, Chronic Illness, and the Physical and Mental Components of the SF-36 Questionnaire. Obes Res. 2000;8:160-70.
- [CrossRef] [PubMed] [Google Scholar]
- Body Mass Index and Subjective Well-being in Young Adults: A Twin Population Study. BMC Public Health. 2013;13:231.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of Psychological Well-being and its Impact on Mental Health In: Issues on Health and Healthcare in India: Focus on the North Eastern Region. Berlin, Germany: Springer; 2018. p. :53-95.
- [CrossRef] [Google Scholar]
- Metabolic Syndrome and Longitudinal Changes in Cognitive Function: A Systematic Review and Meta-analysis. J Alzheimers Dis. 2014;41:151-61.
- [CrossRef] [PubMed] [Google Scholar]
- Cognitive Impairment and Altered Cerebral Glucose Metabolism in the Subacute Stage of COVID-19. Brain. 2021;144:1263-76.
- [CrossRef] [PubMed] [Google Scholar]
- Cognitive Status in COVID-19 Survivors with Metabolic Syndrome. Ser Endocrinol Diabetes Metab. 2021;52:30-8.
- [CrossRef] [Google Scholar]
- Obesity is Associated with Memory Deficits in Young and Middle-aged Adults. Eat Weight Disord. 2006;11:e15-9.
- [CrossRef] [PubMed] [Google Scholar]
- Neuropsychological Function in Individuals with Morbid Obesity: A Cross-sectional Study. BMC Obes. 2017;4:6.
- [CrossRef] [PubMed] [Google Scholar]






