Translate this page into:
Current perception about Leprosy among family members of leprosy patients: A comparative study between high prevalent & low prevalent districts of West Bengal
Address for correspondence: The Editor/ Managing Editor, Journal of Comprehensive Health, Dept of Community medicine, NRS Medical College, 138, AJC Bose Road, Kolkata-700014
Corresponding author: Dr Gitanjali Saha, MBBS, Director, GRECALTES, 35/1A, Old Ballygunge 1st Lane, Kolkata-19 Mobile: 9831189245, email: grecaltes@gmail.com
Abstract
Introduction:
With a sustained effort, India achieved the goal of elimination of leprosy in December, 2005 (PR-0.95/10,000). Since 2001, MDT services in India were integrated with the general health services, thus posing various operational challenges in programme management. With a view to maximize the effectiveness of health education programme, it needs to assess current status of perception and practices of the family members taking care of the patients of the most stigmatized disease so as to adopt appropriate changes accordingly.
Aim(s)/Objective(s):
To assess perception & attitude about leprosy among family members in both high & low endemic districts.
Materials and Method:
25% of leprosy patients getting MDT in 25% blocks of 3 high prevalent & all patients in 25% blocks in 3 low prevalent districts of West Bengal, were initially selected by multi-stage random sampling technique, then family members taking care of the patients, were interviewed.
Statistical Analysis:
Proportions in respect of different attributes calculated & chi-square used as a test of significance.
Results:
Total 246 family members of the leprosy patients, 143 from high prevalent & 103 from low prevalent districts were interviewed. 95.5% & 60.1% of family members respectively have heard about leprosy & MDT. Correct knowledge about cause (38.5% vs 32%), clinical presentation, curability (90% vs 84.5%), infectiousness of the disease(59.4% vs 31%), complication (67.1% vs 52.4%) were found more among family members of high prevalent districts than low prevalent one. 13.59% & 4.2% family members in high & low prevalent districts had belief that leprosy occurred as a result of divine curse. Discrimination towards leprosy patients were found more in low prevalent than high prevalent districts.
Conclusions:
Knowledge & attitude towards leprosy were found to be better among family members in high prevalent as compared to that of low prevalent districts.
Keywords
Leprosy
MDT
Knowledge
attitude
high prevalent
low prevalent.
Introduction:
Leprosy is a disease associated with great societal stigma resulting in discrimination, isolation and injustice.[1,2,3,4] As a result, leprosy patients still delay reporting, becomes defaulter and consequently develop physical deformity.[1,5] With a sustained effort, India achieved the goal of elimination of leprosy in December, 2005 (PR-0.95/10,000). Since 2001, MDT services in India were integrated with the general health services, thus posing various operational challenges in programme management.[6,7]
Early and voluntary reporting is the primary mode of case detection in the post integration era.[8] In sustaining elimination status by general health services, it is required to increase the community awareness and participation, improve capacity building of general health care system, early case detection and early treatment with multi-drug therapy, voluntary reporting of cases, decrease stigma and rehabilitation of leprosy disabled cases.[9]
If the community have negative attitude towards the leprosy patients, then it would force the patients to conceal the disease as long as possible, posing threat to early diagnosis and treatment of the disease. When the disease can no longer be hidden, it would perhaps be too late to prevent deformities, though cure is assured.[10]
It is, therefore, absolutely necessary to make people appropriately aware about leprosy, so that the age old stigma associated with the disease is removed and patients and their family members can easily suspect signs of leprosy and feel free to come forward to the health facilities for early diagnosis and treatment. Through proper spread of IEC and appropriate use of behavioural change communication (BCC), social environment should be made conducive to develop proper attitude towards leprosy at family & community level.
Community participation is an essential ingredient in any successful public health or development programme.[1] Family is the source of social support particularly to the patients who suffer from a chronic & stigmatized disease like leprosy, which is as much a social problem as a medical problem. It was found that knowledge of the affected family about leprosy was significantly associated with their leprosy patient's attendance at treatment clinics.[11] Therefore, Studies on knowledge & attitude on leprosy are essential for understanding the community before starting any meaningful intervention.[6]
In this background, this study was undertaken with the following objectives.
Objectives:
To assess perception & attitude about leprosy among family members of leprosy patients in West Bengal, and
To compare the findings between high & low prevalent districts
Material & Methods:
Type of the Study:
A cross sectional observational study
Settings:
The study was conducted in 3 high prevalent districts (Purulia, Bankura & DakshinDinajpur) and 3 low prevalent districts (Howrah, North & South 24 Parganas) of West Bengal.
Study Subjects:
Family members taking care of the leprosy patients.
Sampling techniques:
Multi-stage sampling technique was adopted
Sample size:
25% of leprosy patients getting MDT in 25% blocks & municipal areas of 3 high prevalent & all patients in 25% blocks & municipal areas in 3 low prevalent districts of West Bengal were initially selected, then the family members taking care of the patients were interviewed.
METHODOLOGY:
In west Bengal Prevalence Rate of Leprosy as on 1st April 2009 was 0.99/10000 population as per Performance Assessment Report of March 2010 under National Leprosy Eradication Program in West Bengal, out of 19 districts, 10 districts have attained elimination status i.e. <1 case per 10000 population, whereas rest of the 9 districts failed to attain this. In the 1st stage sampling, 3 districts from those achieving elimination status and 3 from the rest of the districts were selected randomly for the study. The selected districts in high prevalent areas are Purulia, Bankura & Dakshin Dinajpur and three selected districts in low prevalent areas are Howrah, North & South 24 Paraganas. In the 2nd stage of sampling one -fourth i.e. 25% blocks and 25% of municipality/urban areas (at least one, if total urban area in the district is less than 4) were selected randomly from each selected district. Thus, 13 blocks & 3 municipal areas in high prevalent districts and 18 blocks & 10 municipal areas in low prevalent districts were selected. In 3rd stage of sampling, one fourth (25%) of recorded leprosy patients receiving treatment under NLEP program in each selected blocks of high prevalent districts and all recorded Leprosy patients receiving treatment in each selected block of low prevalent districts were chosen randomly and KAP of one of the family members taking care of the patients was assessed.
Field investigators having exposure to prior field experience in Leprosy work were trained on the schedules to collect data from the study subjects. The schedules developed to collect data was validated independently by three experts working in the field of public health and was pre-tested in similar situation in the field prior to actual survey to rule out operational constraints. Written informed consent was taken from all participants of the study before undertaking interviews. Separate schedule containing open and close ended questions, was used for collecting relevant data from the family members.
Ethical issues:
Ethical clearance was taken from Institutional Ethics Committee of Institute of Post Graduate Medical Education & Research, Kolkata Necessary permission was taken from Dept of Health & Family Welfare to conduct the study in the selected districts and cooperation from the district authority was requested.
Response Variables:
Age, Educational status, Religion, Caste, Socio-economic status, gender, residence, Disease prevalence (high or low), accessibility to health services, accessibility to media, Type of media. Outcome variable: Knowledge, stigma & attitude towards leprosy
Analysis:
Data were entered and analyzed in SPSS 11.5 version. Percentage of positive responses (outcome) was computed with respect to different independent variables and differences in findings between low & prevalent districts were tested by Chi (χ2) test.
Results:
Total 246 family members of the leprosy patients, 143 from high prevalent districts & 103 from low prevalent districts were interviewed. More than 80% respondents were between 20 to 60 years. Majority were female (61.8%) & house-wives (43.9%). 38.2% of family members were illiterate, & 38.6% crossed primary level of education. Illiteracy was found to be more among family members of the patients in high prevalent districts. 84.5% belong to Hindu community and 56.5% were from socially backward classes. About 70 % respondents in high prevalent districts belonged to backward community; the proportion is much higher than that in low prevalent region (39%). 61% were from BPL families. 85% respondents were married. (Table-1)
| Attributes | Categories | High prevalent districts n=143 N0 (%) |
Low prevalent Districts n=103 N0 (%) |
Total N=246 No % |
|---|---|---|---|---|
| Age | 19 and below | 14 (9.79) | 2 (1.94) | 16 (6.50) |
| 20 - 29 | 35 (24.48) | 31 (30.1) | 66 (26.83) | |
| 30 - 39 | 31 (21.68) | 26 (25.24) | 57 (23.17) | |
| 40 - 49 | 26 (18.18) | 20 (19.42) | 46 (18.70) | |
| 50 - 59 | 23 (16.08) | 12 (11.65) | 35 (14.23) | |
| 60 and above | 14 (9.79) | 12 (11.65) | 26 (10.57) | |
| Sex | Male | 58 (40.56) | 36 (34.95) | 94 (38.21) |
| Female | 85 (59.44) | 67 (65.05) | 152 (61.79) | |
| Occupation | At home | 13 (9.09) | 13(12.62) | 26 (10.57) |
| Housewife | 59 (41.26) | 49 (47.57) | 108 (43.90) | |
| Service holder | 35 (24.48) | 29 (28.16) | 64 (26.02) | |
| Student | 9 (6.29) | 5 (4.85) | 14(5.69) | |
| Self employed | 27 (18.88) | 7 (6.8) | 34(13.82) | |
| Education | Illiterate | 68 (47.55) | 26 (25.24) | 94 (38.21) |
| Primary | 50 (34.97) | 45 (43.69) | 95 (38.62) | |
| Secondary | 25 (17.48) | 29 (28.16) | 54 (21.95) | |
| Graduation | 0 (0.00) | 3 (2.91) | 03 (1.22) | |
| Religion | Hindu | 136 (95.1) | 72 (69.9) | 208 (84.55) |
| Muslim | 7 (4.9) | 31(30.1) | 38 (15.45) | |
| Caste | General | 44(30.77) | 63 (61.17) | 107 (43.49) |
| OBC | 10 (6.99) | 5 (4.85) | 15(6.10) | |
| SC | 69 (48.25) | 33 (32.04) | 102 (41.46) | |
| ST | 20 (13.99) | 2 (1.94) | 22 (8.94) | |
| Economic status | APL | 46 (32.17) | 49 (47.57) | 95 (38.62) |
| BPL | 97 (67.83) | 54 (52.43) | 151(61.38) | |
| Marital Status | Married | 122(85.31) | 87(84.47) | 209(84.96) |
| Unmarried | 16 (11.19) | 10 (9.71) | 26 (10.57) | |
| Others | 5 (3.5) | 6 (5.82) | 11 (4.47) |
95.5% of family members have heard about leprosy. 35.8% respondents have correct knowledge that it was caused by bacteria, whereas 34 % have no idea about the cause of disease. 38.5% members in high prevalent areas have correct knowledge regarding causal agent compared with those from low prevalent areas (32%). 36.2% respondents answered that through cough & sneezing leprosy could spread. That close contact and sharing articles with patients could transmit leprosy were the response from 13% & 17.5% family members respectively. Most of the respondents identified anaesthetic patch (45.9%) or hypo-pigmented patch (33.7%) to be the main presenting sign. About 70% respondents have knowledge about at least one presenting sign of leprosy (hypopigmented patch, anesthetic patch or thickened nerve). Those from high prevalent districts have better knowledge than their counterparts in low prevalent districts (75.5% vs 62.1%). Correct response regarding infectiousness of the disease was found more among family members of leprosy patients from high prevalent districts (59.4%) than low prevalent one (31%), the difference was found to be statistically significant.(p=.00001). Most of the family members, 90% in high endemic area & 84.5% in low endemic area were aware that leprosy was curable. 60.1 % family members heard about MDT. The proportion seemed to be higher among family members belonging to high prevalent community than that of low prevalent one. 41.8% family members, more in low prevalent districts, have the correct knowledge about time required to complete leprosy treatment. (Table-2, Fig 1)

- Proportion of family members having correct knowledge about leprosy in high & low prevalent districts.
| Attributes | Response | High prevalent districts n=143 N0 (%) |
Low prevalent Districts n=103 N0 % |
Total N=246 N0 % |
χ2 p |
|---|---|---|---|---|---|
| Heard about leprosy | Yes | 135 (94.41 | 100 (97.09) | 235 (95.53) | 1.01 .31 |
| No | 8(5.59) | 3 (2.91) | 11(4.47) | ||
| Cause of leprosy | Correct | 55 (38.46) | 33(32.04) | 88 (35.77) | 1.07 0.299 |
| Incorrect | 88(61.54) | 70(67.96) | 158(64.23) | ||
| Mode of spread | Correct | 53(37.06) | 36 (34.95) | 89 (36.18) | 0.11 0.73 |
| Incorrect | 90(62.94) | 67(65.35) | 157(63.82) | ||
| Signs of leprosy | Correct (at least one sign) | 108(75.52) | 64(62.14) | 172(69.92) | 5.1 .02 |
| Incorrect | 35(24.48) | 39(37.86) | 74(30.08) | ||
| Infectiousness to others | Correct | 85 (59.44) | 32 (31.07) | 117 (47.56) | 19.3 .00001 |
| Incorrect | 58(40.56) | 71(68.93) | 129(52.44) | ||
| Is leprosy curable? | Yes | 129 (90.21) | 87 (84.47) | 216 (87.80 | 1.84 .17 |
| No | 3 (2.1) | 5 (4.85) | 8 (3.25) | ||
| Don't know | 11 (7.69) | 11 (10.68) | 22 (8.94) | ||
| Heard about MDT | Yes | 92 (64.34) | 58 (56.31) | 150 (60.98) | 1.62 .20 |
| No | 51(35.66) | 45 (43.69) | 96(39.02) | ||
| Duration of treatment | Correct | 51(35.66) | 52(50.49) | 103(41.87) | 5.4 .02 |
| Incorrect | 92 (64.34) | 51(49.51) | 143(58.13) |
77.2% family members have preference for MO or health workers for early consultation for the disease. Similarly, either hospital or sub-centre (91%) was their preferred place for treatment. (Fig-2)
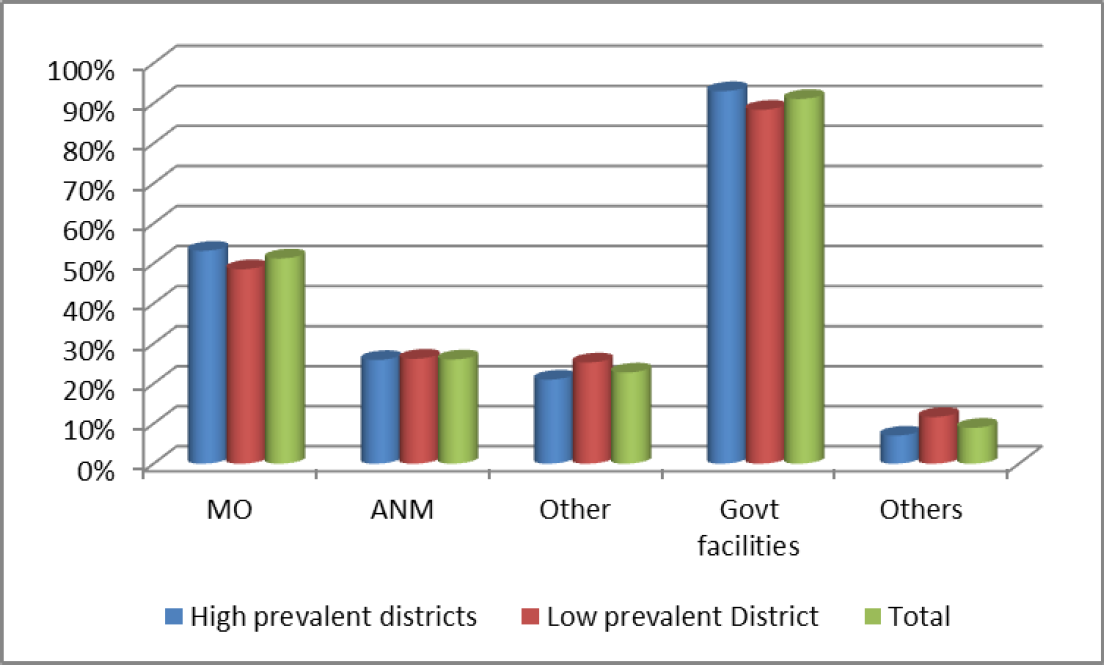
- Proportion of respondents showing preferences of consultation for leprosy
Most of the family members (61%) mentioned deformity as a complication of leprosy, this idea was found more prevalent in high endemic (67.1%) than low endemic districts (52.4%). 14.3% family members considered ulcer to be another form of complication of leprosy. 92.3% family members have the idea that early diagnosis & treatment would cure leprosy completely, but few persons (5.3) still have the faith that worshiping God was the remedy of leprosy. This faith was more prevalent in low endemic areas (10.7%) compared with high endemic one (1.4%). (Table-3)
| Attributes | Categories | High prevalent districts n=143 N0 (%) |
Low prevalent Districts n=103 N0 % |
Total N=246 No % |
|---|---|---|---|---|
| What are the complications of leprosy, if not treated? | Deformity | 96 (67.13) | 54 (52.43) | 150 (60.97) |
| Ulcer | 20 (13.99) | 16 (15.53) | 36 (14.63) | |
| Others | 8 (5.59) | 25 (24.27) | 33 (13.41) | |
| Don't know | 20 (13.99) | 19 (18.45) | 39 (15.85) | |
| How should a patient avoid disability? | Early diagnosis and treatment with MDT | 133 (93.01) | 94 (91.26) | 227 (92.28) |
| Worshiping God | 2 (1.4) | 11(10.68) | 13 (5.28) | |
| Don't know | 8 (5.59) | 10 (9.71) | 18 (7.32) |
Major sources of information were found to be radio (23.2%), hoarding (22.76%) & TV (39.4%). People from low prevalent districts (55.3%) got information mostly from television. Family members in the study area got information about leprosy primarily from Health workers (44.3%), Medical Officers (18.3%) and neighbours (16.7%). Compared to the low prevalent districts, majority of the family members in high prevalent districts got information about leprosy from health workers (ANM) (51% vs 34.95%) & ASHA (15.38% vs 3.88%)).
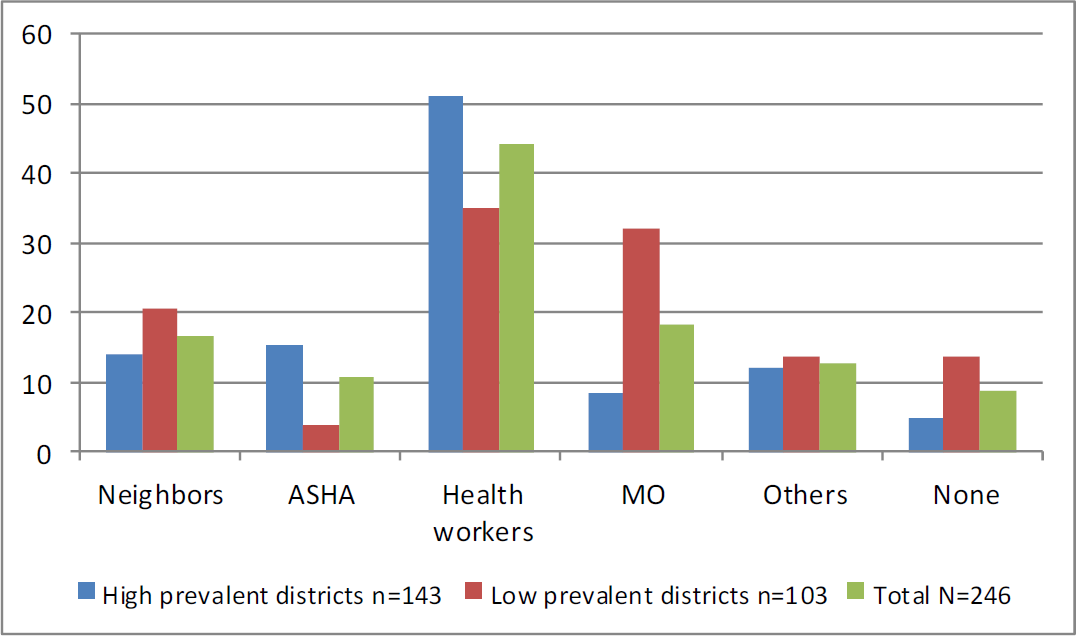
- Proportion of respondents getting information from individuals
Though 78% family members did not believe that leprosy occurred as a result of divine curse, 8.1% family members had such belief, which was more prevalent in low prevalent districts (13.59%) compared with high prevalent one (4.2%). 14.6% family members considered that leprosy was the result of patients' own fault/misdeed. This belief, similarly, more predominant among family members in low endemic districts (21.36%). 17% respondents expressed their opinions that leprosy patient should be kept away from family members & community. Though 91.9% family members did not discriminate with the patient, 4% were showing such discrimination. This was found more in low prevalent areas (5.8%). Only 0.7% respondents in high prevalent districts and 5.8% in low prevalent districts said that they had experienced discrimination from society. 9.3% family members did not allow leprosy patients to share the room with other members of the family, this proportion was 12.6% in low prevalent districts compared with high prevalent districts where the proportion was 7%, the difference was found to be significant.(Table 4)
| Attributes | Categories | High prevalent districts n=143 N0 (%) |
Low prevalent Districts n=103 N0 % |
Total N=246 No % |
|---|---|---|---|---|
| Do you consider the disease as a curse of God?* | Yes | 6 (4.2o) | 14 (13.59) | 20(8.12) |
| No | 116 (81.12) | 76 (73.79) | 192 (78.05) | |
| Don't know | 21 (14.69) | 13 (12.62) | 34(13.82) | |
| Do you consider the disease as own fault of the patient?* | Yes | 14 (9.79) | 22 (21.36) | 36 (14.63) |
| No | 98 (68.53) | 61 (59.22) | 159 (64.63) | |
| Don't know | 31 (21.68) | 20 (19.42) | 51(20.73) | |
| Should a patient of leprosy separated from other member of family/community? | Yes | 21(14.69) | 21 (20.39) | 42 (17.07) |
| No | 113 (79.02) | 78 (75.73) | 191(77.64) | |
| Don't know | 9 (6.29) | 4(3.88) | 13 (5.28) | |
| Have you made any discrimination to the patient? | Yes | 4 (2.8) | 6 (5.83) | 10 (4.06) |
| No | 132 (92.31) | 94 (91.26) | 226(91.87) | |
| Don't know | 7 (4.90) | 3 (2.91) | 10 (4.06) | |
| Have your family faced any discrimination?* | Yes | 1 (0.7) | 6 (5.83) | 7 (2.84) |
| No | 135 (94.41) | 93 (90.29) | 228 (92.68) | |
| Don't know | 7 (4.90) | 4 (3.88) | 11 (4.47) | |
| Do the patient live in the same room with other family members? | Yes | 126 (88.11) | 88 (85.44) | 214 (86.99) |
| No | 10 (6.99) | 13 (12.62) | 23 (9.35) | |
| Didn't answer | 6 (4.2) | 2 (1.94) | 8 (3.25) |
*p< .05
Discussion:
In this study, it is found that correct knowledge of family members of leprosy patients about cause of disease and mode of spread were 35.8% and 36.2% respectively. About 48% have idea that, not all, but few patients are infectious to others. Most of the respondents identified anaesthetic patch (45.9%) or hypo-pigmented patch (33.7%) to be the main presenting sign. About 70% respondents have knowledge about at least one presenting sign of leprosy (hypopigmented patch, anesthetic patch or thickened nerve). Most of the family members (87.8%) were aware that leprosy was curable and about 61% heard about MDT, but less number (41.8%) were aware about time required to complete leprosy treatment. 61% and 14.3% of family members mentioned deformity and ulcer respectively as complication of leprosy, and majority (92.3%) of them mentioned that early diagnosis & treatment would cure leprosy completely.
A qualitative study conducted in Tamilnadu on people's understanding and behaviour towards leprosy and patients, revealed similar findings. Most of the respondents, both leprosy patients and the community women did not have proper knowledge on cause, mode of spread and prevention of leprosy. Instead they had misconceptions about cause and spread.[10] Another study conducted in Uttar Pradesh by Barkataki et al in 2006 reported that less than 10% of illiterates and about 40% of literates cited infection as the cause of leprosy.[12]
A study conducted on leprosy patients and their family members in a rural community in Tamilnadu revealed more or less similar findings. Regarding the knowledge level of leprosy, about 37% of family members were aware that leprosy is due to infection caused by a germ. Regarding the presenting symptoms, about 73% of family members said that patches on the skin and loss of sensation were important symptoms of leprosy. Regarding the mode of spread, about 45% of the family member also said leprosy is spread through air. 64% of family members responded correctly for duration of treatment of leprosy. Regarding cure of leprosy, 64% of family members answered in the affirmative that leprosy is curable.[11] Community views on leprosy in Tamilnadu reveals that Knowledge and awareness of leprosy with respect to cause for getting leprosy, more than half of them said that they did not know the cause and some, mentioned that leprosy is hereditary. With respect to the spread of the disease, most of them were unaware of the same.[10]
As a result of continuing effort by government & non-government agencies working in the field, stigma & discrimination have been reduced over the time, current study stilled revealed some adverse ideas among family members of leprosy patients. Though 78% family members did not believe that leprosy occurred as a result of divine curse, 8.1% family members had such belief, 14.6% family members considered that leprosy was the result of patients' own fault/misdeed. 17% respondents considered that leprosy patient should be kept away from family members & community, and, 5.3% of respondents still have the faith that worshiping God was the remedy of leprosy. Though 91.9% family members did not discriminate with the patient, 4% were showing such discrimination. 9.3% family members did not allow leprosy patients to share the room with other members of the family.
Findings of focus group discussion (FGDs) conducted in the same settings, identified stigma and adverse attitude among villagers (114 villagers took part in different groups). A high proportion of them expressed their opinion that leprosy patients should not be allowed to move freely in the community or to attend any social events.[13]
Stigma & misconception are age old problems found to be associated with leprosy. Different studies done in India & abroad revealed the same findings.[11,12,14,15] Tamilnadu study showed that all the patients felt the need for discrete form of treatment [not revealing to others] and 82% of the family members said that a leprosy patient can stay with them in their house and 73% of them hesitated to share articles of leprosy patient. 91% of the family members felt that leprosy patients can be employable and doesn't mind sitting beside them. Regarding the right attitude, the average score was only about 41% favorable for the patients and 67% favorable for the family members towards the disease.[11]
In a study (Barkataki et al 2006) [12] undertaken in Uttar Pradesh among leprosy patients and community members, it was reported that nearly 50-60% community members stated that there was discrimination. Nearly 70% felt that leprosy affected social participation, over 90% attributing this to adverse social stigma. Stigma at workplace, sometimes at home and in community was found in brazil.[14] In Brazil, in one study, most (55%) of the participants (patients) said that there had seen behavioural changes in their family members when they were diagnosed as having leprosy.
Specifically, there were reactions of religiosity, prejudice, guilt, fear and escape.[15] The study revealed that knowledge of family members of leprosy patients from high prevalent districts regarding different aspects of leprosy were better than their counterparts from low prevalent districts, difference with respect to signs of leprosy and infectiousness to other people was statistically significant. Similarly, stigma related to leprosy making negative attitude was found more among family members of low prevalent districts. On further enquiry, it was found that in high prevalent districts, family members got information mostly from ANM & ASHA, whereas those of low prevalent districts got information mostly from Television.
Similar findings were noted in the same settings which revealed that KAP of leprosy patients of low endemic districts were found much less that of high endemic one and more proportion of MB cases & disabilities were found there. Comparatively high proportion of patients with disability were found to be uncared.[16]
As being high prevalent districts, workers were probably more oriented, had good contact with family of leprosy patients. Improved picture with greatly reducing stigma & discrimination and elevated knowledge in the high prevalent district have been possible as a result of continuing effort made by government health system as well as effort of NGO working there over a long period of time. People from low prevalent districts were found to be more stigmatised needing continuous IEC campaign including inter-personal communication.
Conclusion & recommendation:
Knowledge & attitude towards leprosy were found to be better among family members in high prevalent as compared to that of low prevalent districts.
Low prevalent districts should be given equal importance in IEC activities to remove stigma, discrimination and fear about leprosy so that family members feel free to communicate with health facilities for early diagnosis and treatment and also play supportive role and create enabling environment in patient care.
Acknowledgment:
We gratefully acknowledge the financial support made by the Indian Council of Medical Research, New Delhi for the Original Research Work entitled: “Current Knowledge, Attitude and Practices (KAP) about Leprosy among Leprosy Patients, their family members, Service Providers and General Populations; a comparative study between high prevalent & low prevalent districts of West Bengal”. We are indebted to Dr Vishwa Mohan Katoch, Former Director General, ICMR and Former Secretary, Department of Health Research, Govt of India for his contribution to conduct this study. We are equally thankful to the Department of Health & Family Welfare, Government of West Bengal for providing data regarding leprosy patients under treatment, and the patients & family members for their cooperation.
Reference:
- A Study on Community-based Approaches to Reduce Leprosy Stigma in India. Indian J Lepr. 2008;80:267-273.
- [Google Scholar]
- Qualitative assessment of social, economic and medical needs for ex-leprosy patients living in leprosy villages in Shandong Province, The People's Republic of China. Lepr Rev. 2005;76:335-347.
- [CrossRef] [PubMed] [Google Scholar]
- A study on knowledge, beliefs and attitude towards leprosy in students of Jaipur, Rajasthan. Indian J Lepr. 2012;84:277-285.
- [Google Scholar]
- Delay in presentation and start of treatment in leprosy patients : a case-control study of disabled and non-disabled patients in three different settings in Ethiopia. Int J Lepr Other Mycobact Dis. 1998;66:1-9.
- [Google Scholar]
- Effect of Environment and Education on knowledge and attitude of nursing students towars leprosy. Indian J Lepr. 2011;83:37-43.
- [Google Scholar]
- Determinants of rural women's participation in India's National Leprosy Eradication Programme. Indian J Lepr. 2014;86:105-110.
- [Google Scholar]
- Increased need for health education and communication services in contemporary practice. Indian J Lepr. 2012;84:321-322.
- [Google Scholar]
- Knowledge and work performance of multipurpose workers under national leprosy eradication programme in Satara District, Maharastha. Indian J Lepr. 2012;84:137-144.
- [Google Scholar]
- Awareness, social acceptance and community views on leprosy and its relevance for leprosy control, Tamil Nadu. Indian J Lepr. 2012;84:233-240.
- [Google Scholar]
- Assessment of Knowledge, Attitude and Practice about leprosy among patients and their families in a rural community in Tamil Nadu. Indian J Lepr. 2014;86:7-14.
- [Google Scholar]
- Knowledge of and attitudes to leprosy among patients and community members: a comparative study in Uttar Pradesh, India. Lepr Rev. 2006;77:62-68.
- [CrossRef] [PubMed] [Google Scholar]
- A Qualitative Assessment of Current Perception of Different Social Groups about Leprosy in High & Low Prevalent Districts of West Bengal. Journal of Comprehensive Health. 2015;3(2) (accessed )
- [CrossRef] [Google Scholar]
- Satisfaction of leprosy patients on integrated MDT services as evaluated by Batgarh integrated community health project (BICHP) Indian J Lepr. 2011;83:53-59.
- [Google Scholar]
- Leprosy as a Neglected Disease and Its Stigma in the Northeast of Brazil. Indian J Lepr. 2014;86:53-59.
- [Google Scholar]
- Current Perceptions and Practices (KAP) about Leprosy among Leprosy Patients: A Comparative Study between High Prevalent & Low Prevalent Districts of West Bengal. Indian J Lepr. 2015;87:1-16.
- [Google Scholar]






