Translate this page into:
Structural Vulnerability and Epidemiology of COVID-19 in India- A Socio-epidemiological Approach for Health Promotion
Corresponding author: Dr. Monalisha Sahu, Assistant Professor (Public Health), Dept of Health Promotion & Education, Room no. 305, All India Institute of Hygiene and Public Health. 110, Chittaranjan Avenue, Kolkata - 700073, E mail: drmonalisha@outlook.com, Mobile no. (+91) 9873927966
How to cite this article: Sahu M, Dobe M,Yadav K. Structural Vulnerability and Epidemiology of COVID-19 in India- A Socioepidemiological Approach for Health Promotion. J Comprehensive Health 2020;8(2): 60-65.
Abstract
Introduction:
COVID-19 (2019 Novel Coronavirus) pandemic is an outcome of a "complex system" of interactions occurring within and between individuals and their environments. The individual-level models, which give sole or primary emphasis to individual choice with their "victim blaming" tendency is insufficient as determinants of risk and risk behaviour. There are 'structural vulnerabilities' that are likely to lead to increased exposure to the contagion, risk of basic human needs not being met, insufficient support, or inadequate treatment
Objective:
To explore various structural vulnerabilities affecting spread and responses to COVID-19 pandemic.
Method:
We have conducted a scoping review of secondary data and statistics on COVID-19 from January 2020 to July 2020 in context of various structural vulnerability across various states and Union Territories of India.
Result:
It was observed that individuals had dynamic and reciprocal association with their physical social, political and economic environments significantly modifying their vulnerabilities to the disease. We classified the various social vulnerabilities majorly faced by individuals into three domains: a) Socio demographic composition b) Spatial distribution across various States and Union territories and c) Migration. It was observed that elderly and male gender were more prone to death by COVID-19 whereas children were found to be less susceptible to the disease. Individuals with underlying illnesses such as cardiovascular diseases (death rate 13.2%), diabetes (death rate 9.2%), high blood pressure (death rate 8.4%), and chronic respiratory diseases (death rate 8%) were at significantly higher risk of mortality. Though the states and cities with maximum connectivity and population density (like Mumbai, Delhi) were afflicted most in the early days of pandemic, but with reverse migration the virus manged to reach even the deepest hinterlands of the country.
Conclusion:
For an efficient response towards the COVID-19 pandemic it is important for policy makers to look through the lens of structural vulnerability and formulate relevant Socio-epidemiological approach.
Keywords
Structural vulnerability
Socio epidemiological
COVID19
Coronavirus
Framework.
Introduction
COVID-19 is an unprecedented challenge; ripping off the already compromised health systems of developing countries like never before. Whilst everyone is potentially at risk of harm in this pandemic, there is a social gradient to the risk; making some segments of the population more vulnerable and at a heightened risk of infection.
'Structural vulnerability' is a concept used to understand how the social determinants of health translate to the poor health outcomes faced by individuals.[1] The concept suggests that because of the unequal positions of individuals and groups in society, they may face greater exposure to risk, their ability to live healthy lifestyles and adopt precautionary behaviour and they may be unable to access and afford health care when they need it.[1,2]
Although there is a rich theoretical and empirical tradition in the social sciences for investigating health as an effect of social inequality and conditions; public health has not dialogued systematically with social science theories and methods.[3,4] However, to understand how differential social circumstances can transform ongoing COVID-19 pandemic and result in exacerbated health problems for vulnerable individuals, an iterative and multidisciplinary approach is required. A synthesis of social and epidemiological approaches thus, seeks to delineate how the distribution of the COVID infection in populations is shaped by the "risk environment," that is, by determinants that extend beyond "proximal" individual-level factors and their behavioural mediators.[4]
Taking this in consideration this study was conducted with the objectives of to determine how Structural Vulnerability is impacting on the risk of COVID-19 pandemic in India and Aim of the study was to explore various structural vulnerabilities affecting spread and responses to COVID-19 pandemic.
Methods
We have done a scoping review taking in account data from various States and Union territories of the country where the outbreak of this virus has become a substantial problem. In each state, the number of COVID-19 Confirmed Cases and deaths are taken into consideration. We considered the following three domains: a)Socio demographic composition (Age, gender, social stratification, associated comorbidities), b)Migration, and c)Spatial distribution with state differentials in the context of the structural vulnerability for COVID-19 epidemic in India, particularly for management and mitigation of COVID-19 infection in the community. The study period incorporates all relevant information since the outbreak of this epidemic in India from 30th January,2020 up to the July 14, 2020. The data incorporated in this study includes all scientific information reported up to the latest of July 14, 2020 that includes Ministerial reports, journal articles and newspaper reports. Our objective was to explore how social structures generate and reproduce structure vulnerability to COVID-19 infection. We, therefore, outlined a case for a "social epidemiology of structural vulnerability" to illustrate the relevance of these concepts in the COVID-19 risk environment.
We have used Microsoft Excel and Data wrapper software to generate tables and maps in this review.
Results
While studying the contributions of all three domains of socio demographic composition (Age, gender associated comorbidities and social stratification), migration and spatial distribution with state differentials in explaining the vulnerability and responses to COVID-19, following findings were noted:
A) Socio Demographic Composition
Age group:
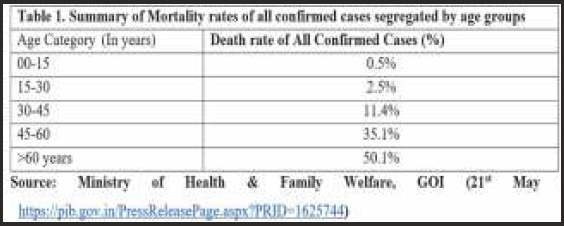
While Young Indians were at higher risk of contracting the disease as about 60 per cent of the patients were under the age of 50 in India; senior citizens were more prone to death by COVID-19, as 75.3% of the COVID-19 deaths belonged to above 60 yrs. age category. 5 Further age wise categorization of mortality data has been represented in Table No.1. Children were found to be less susceptible to the disease. WHO has also reported the highest worldwide mortality among people over 80 years of age whereas adults younger than a 60 yrs. of age were less likely to die from it.[6] As less than 10% of Indian population is above 60 years of age, so mortality rate in relatively younger population seems to be higher in India as compared to European countries, where the proportion of population above 60 is relatively high.[5,7]
Gender: In India, the trends currently suggest that 76% of the reported cases were reported in males. Also, 73% of the reported mortalities due to COVID 19 were among males. 8 This trend first seen in China, has been mirrored in Iran, South Korea and European countries like Italy France, Germany and now in the UK. It can be partially blamed upon higher prevalence of smoking and travelling in men. Furthermore, the Lockdown to ensure social distancing has also increased the incidences of violence against women to a larger extent which also leads to abandonment of "staying at home". Also, females are more likely to adopt preventive behavioural and hygienic measures and health-seeking behaviours. However, plausibility of a biological gendered impact can't be totally denied.[8,9]
Co-morbidities:
Researchers around the world have suggested that most fatalities have been reported amongst those with underlying illnesses such as cardiovascular diseases (death rate 13.2%), diabetes (death rate 9.2%), high blood pressure (death rate 8.4%), chronic respiratory diseases (death rate 8%) and cancer (death rate 7.6%) while death rates were as low as 0.9% in people with no pre-existing conditions.[10] The high death rate of COVID-19 was more related to age group above 50, and those with cardiovascular diseases.[11] In India 83% of the deceased had reported co- morbidities.5 More than 40% of the cases examined had two pre-existing disease conditions, while over 17% had more than three co-morbidities. Only about a third of those who died (35%) had just one co-morbidity.[12] Unlike rest of the world, most common co-morbidities among those who died of Covid-19 in India so far had either diabetes or hypertension, and in a large number of cases both conditions were present together.
Social stratification of COVID-19: The pandemic of COVID-19 is not an equalizer; rather it has shone a harsh light on inequality making social stratification even more apparent. Stark gaps in wealth, health and work have gone from being chronic problems to acute ones. There are wide gaps by income class in both the risk posed by the virus, because of existing health conditions, and in levels of response to the risk of infection amplifying the impact of the virus and raise mortality rates.
The lower social strata, as the most vulnerable section of society, are bearing the brunt of adverse social and economic outcomes posed by COVID -19 making them much more vulnerable to the disease as well as face significant barriers in seeking care.[13] India also has a higher risk of community transmission because of crowded living conditions, high levels of poverty, a large slum-dwelling population lacking basic sanitation and poor health-care facilities.
The country went into world's largest lockdown on March 25, 2020, restricting 1.3 billion people for maintaining adequate social distance to stop spread of the disease. The lockdown made it harder for the lower strata. To maintain social distancing, social security is the pre requisite. It needs availability of soap and water to wash hands properly to practice hand hygiene. The concept of social distancing does not squarely apply to the reality of urban slums or other cramped/overcrowded places. The scale, speed, and the extent of these sovereign measures were uneven and showed the uneven capacity of the states to decide whether to give priority to economy or to life. This unevenness of state capacity to respond to Covid-19 highlighted a long-term failure to sustain public health and life.
B) Migration:
The Cross-border migration is a visible reflection of global inequalities. Migrants are forced to leave their native places in search of better opportunities and earnings, many times leaving behind their families. The total number of internal migrants (inter- and intra-state movement) in India is a staggering 139 million[14]. After India announced a nationwide lockdown to contain the spread of the coronavirus, thousands of migrant workers lost their livelihood and, in an attempt, to return their origin districts gathered near railway station, defying rules of social distancing, putting themselves and others at risk[15].
Many of them were stranded and had no option than live under unhygienic and hazardous conditions. Though the Government tried to provide basic amenities like shelter, water, sanitation, toilets, and food; the benefits didn't reach all of them may be because of an inefficient outreach or policymakers' myopia. They became highly prone to various social, psychological and emotional trauma in prevailing situations, emanating from fear of the disease, neglect by the local community and concerns about wellbeing and safety of their families waiting in their native places making scores of migrant workers to move back to their native places using all possible means. In the first 3 weeks of May, Indian railways alone ferried around 4 million migrant workers to their states of origin.
Most of these people travelled to Uttar Pradesh and Bihar, followed by Madhya Pradesh, Punjab, Rajasthan, Uttarakhand, Jammu and Kashmir, and West Bengal. An important issue here is that most of these migrant workers active cases; eg, Delhi, Maharashtra, Tamil Nadu, Gujarat, Andhra Pradesh, and Kerala) to lower-burden but highly vulnerable districts in their own states, possibly carrying back infection, increasing threat of virus spreading in their districts. C) Spatial distribution & State differentials: Diseases like COVID 19 move quickly between people. However, the exposure behaviour of each disease differs from another depending on regional or space factors and environmental conditions. As of July 5, 2020, in India, more than 648 300 confirmed cases have been reported, of which around 235 433 (36%) were active, 394 227 (61%) recovered, and 18 655 (3%) died.2 These cases were spread over 35 (97%) of 36 states and union territories and 627 (98%) of 640 districts of the country.

Comparative analysis of distribution of confirmed COVID 19 cases and deaths in beginning of the pandemic in India and in the current situation across the various states and Union territories in India has shown emergence of new hotspots [Figure. 1]. Early in the pandemic, by end of April 2020 the western state of Maharashtra was the worst hit state with 8,590 cases and 369 deaths. Maharashtra is the largest are returning from states with a high burden (in terms of urbanization in the country, close to the Mumbai financial centre and the stock market. The western state of Gujarat and the capital city of Delhi trailed behind at 3,548 and 3,108 cases, respectively. At 1,760 active cases, Madhya Pradesh has the fourth-highest number of active cases, followed by Rajasthan (1,626). The top five states together account for 70 percent of the active cases nationally, and the top ten states account for 91 percent of all cases. The states of Sikkim and Nagaland, and Union Territories of Daman & Diu, Dadra & Nagar Haveli and Lakshadweep were yet to report any COVID19 case. West Bengal, Maharashtra and Gujarat saw the highest spike in cases among top ten states with most cases. These three states account for 65 percent of all the new active cases in this period.
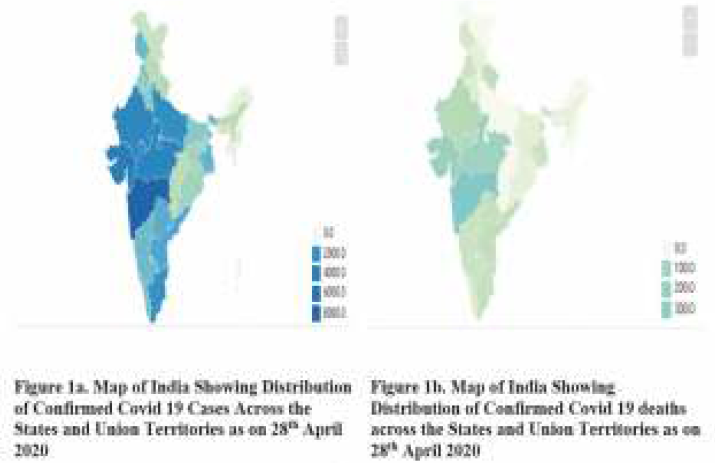
- Map of India showing distribution of cases and deaths across various states and Union territories (as on 28th April, 2020 vs as on 14/07/2020)

Mumbai, Ahmedabad, New Delhi, Indore and Krishna districts-These five districts accounted for 49 percent of new cases over this period. Other districts that saw a sharp spike lately included Kolkata, Chennai, and Surat.[16,17]
Presently, the disease has begun to spread from large cities to smaller towns and rural areas after overwhelming the megacities. Initially isolated from the epidemic, rural areas were exposed when millions of migrant workers who lost their jobs in the cities due to the lockdown returned to their homes. Though Maharashtra is still reporting the highest number of infections, followed by Tamil Nadu, Delhi, Karnataka and Gujarat. The states like Karnataka, Bihar, Andhra Pradesh, Odisha, Uttar Pradesh and Telangana are emerging as the states where the virus is spreading at the fastest pace right now with doubling time lesser than national average. Cities like Ahmedabad, Bhopal, Indore have witnessed a sudden spike, mainly because of congested urban settlements. Even Kerala, which had controlled the outbreak, and states like Jharkhand and Assam have shown spikes with rapid growth in numbers.
If the disease spreads in rural areas which have much weaker health system in proportions similar to in megacities, the adverse health effects are likely to be far more catastrophic. Based on all these findings we are proposing a simplified framework of present and future structural vulnerabilities and their effect on COVID-19 pandemic in India.[Figure. 2]

- A Simplified Framework of Structural Vulnerability and its impact on the COVIC19 pandemic in India.
Conclusion
The health of individuals and communities is an embodiment of their social condition and so the health improvement essentially requires social and structural change. Hence, we advocate for a paradigm shift "from the individual to the social" approach of preparedness in public health emergencies. In this regard, incorporating a well-designed fiscal stimulus package, prioritizing health spending to contain the spread of the virus and providing income support to households most affected by the pandemic would help to contain the contagion as well as minimize the likelihood of a deep economic recession.
There is connection between communities that experience disparities during non-emergency times and their ability of resilience to rally from pandemics.
As events unfold, we need to see opportunities to explore scenarios, improve policies and fast-track policy options for migrants that have already been discussed for some time.
The prioritization and progress of marginalised communities and populations is key to disaster risk reduction. As with the Sendai Framework, setting four specific priorities for action: Understanding risk not only from individual but also the social perspective; Investing in risk reduction for increasing social resilience during preparedness phase; Enhancing preparedness for effective response, and to a robust plan to "Build Back Better" during recovery; aligning with and reaffirming sustainable development goals (SDG) is the need of the hour.
Acknowledgement:
Ministry of Health & Family Welfare & John Hopkins University for COVID related data and updates. We are also thankful to Dr Shyambhavee, Senior Resident RML Hospital for providing her valuable insights
Conflict of Interest:
Nil
Source(s) of support:
Nil
References:
- Structural vulnerability: operationalizing the concept to address health disparities in clinical care. Academic medicine: journal of the Association of American Medical Colleges. 2017;92(3):299-307.
- [CrossRef] [PubMed] [Google Scholar]
- The determinants of health: structure, context and agency. Sociology of Health & Illness. (3):131-54.
- [CrossRef] [Google Scholar]
- Transforming social structures and environments to help in HIV prevention. Health Affairs. 2009;28(6):1655-65.
- [CrossRef] [PubMed] [Google Scholar]
- Structural violence and structural vulnerability within the risk environment: theoretical and methodological perspectives for a social epidemiology of HIV risk among injection drug users and sex workers. Rethinking Social Epidemiology: Towards a Science of Change. Chapter 10. 2012:p205-230.
- [CrossRef] [Google Scholar]
- Government of India. Updates on COVID-19 Available from: https://pib.gov.in/PressReleasePage.aspx?PRID=1615800 (accessed ) (accessed )
- [Google Scholar]
- Statement - Older people are at highest risk from COVID- 19, but all must act to prevent community spread. Available from: http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid- 19/statements/statement-older-people-are-at-highest- risk-from-covid-19,-but-all-must-act-to-prevent-community-spread (accessed ) (accessed )
- [Google Scholar]
- Available from: http://censusindia.gov.in/Ad_Campaign/press/DataHighlghts.pdf (accessed ) (accessed )
- Government of India. Updates on COVID-19 Available from: https://pib.gov.in/PressReleasePage.aspx?PRID=1625744 (accessed )
- [Google Scholar]
- Global Health 5050. Towards gender equality in global health. Available from: https://globalhealth5050.org/covid19/ (accessed ) (accessed )
- [Google Scholar]
- Clinical features of deaths in the novel coronavirus epidemic in China. Rev Med Virol 2020:e2103.
- [CrossRef] [PubMed] [Google Scholar]
- World Health Organization. 2020 February Available from: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf (accessed ) (accessed )
- [Google Scholar]
- Average age of India's Covid deaths 60; diabetes, BP common co-ailments. The Times of India. [Internet] 2020 April 8 India News. Available from: https://timesofindia. indiatimes.com/india/average-age-of-indias-covid- deaths-60-diabetes-bp-common-co-ailments/ articleshow/75037820.cms?utm_source=contentofinter est&utm_medium=text&utm_campaign=cppst (accessed ) (accessed )
- [Google Scholar]
- Department of Economic and Social Affairs. Social Inclusion. Available from: https://www.un.org/development/desa/ dspd/everyone-included-covid-19.html (accessed ) (accessed )
- [Google Scholar]
- India has 139 million internal migrants. They must not be forgotten. [Internet] World Economic Forum 2017 October 1 Available from: https://www.weforum.org/agenda/2017/10/india-has-139-million-internal-migrants-we-must-not-forget-them/ (accessed ) (accessed )
- [Google Scholar]
- COVID-19 and India's Nowhere People. The lockdown, and loss of jobs, lays bare the plight of India's millions of internal migrants [Internet] The Diplomat 2020 April 01 Available from: https://thediplomat.com/2020/04/covid-19-and-indias-nowhere-people/ (accessed ) (accessed )
- [Google Scholar]
- COVID-19 and India's Nowhere People. The lockdown, and loss of jobs, lays bare the plight of India's millions of internal migrants [Internet] 2020 April 01 The Diplomat. Available from: https://thediplomat.com/2020/04/covid-19-and-indias- nowhere-people/ (accessed ) (accessed )
- [Google Scholar]
- Mint COVID Tracker: Half of all new cases in Mumbai, Ahmedabad, New Delhi, Indore, Krishna districts. Livemint. [Internet] In: India [about 3 pages]. 2020. Available from: https://www.livemint.com/news/india/mint-covid-tracker-half-of-all-new-cases-in-mumbai-ahmedabad-new-delhi-indore-and-krishna-districts-11588045302144.html (accessed ) (accessed )
- [Google Scholar]
- Maps and Trends. Mortality Analysis [Internet] Available from: https://coronavirus.jhu.edu/data/mortality (accessed ) (accessed )
- [Google Scholar]






