Translate this page into:
Risk factor profile of stroke patients with special focus on determinants of severity
Address for correspondence: The Editor/ Managing Editor, Journal of Comprehensive Health, Dept of Community medicine, NRS Medical College, 138, AJC Bose Road, Kolkata-700014
Corresponding author: Dr. Zinia T. Nujum, Associate Professor (CAP), Department of Community Medicine, Govt. Medical College, Thiruvananthapuram, P. O, Thiruvananthapuram, Kerala, India - 695011. Phone numbers: 9037356908, E-mail address: drzinia@gmail.com
Abstract
Background:
Stroke is the second major cause of death worldwide and the fourth major cause of death in India. Kerala is becoming the hotspot of lifestyle diseases. Almost 90% of the cases reported in Kerala are associated with one or two modifiable risk factor(s) in the form of lifestyle diseases.
Objectives:
This study is aimed at risk factor profiling of stroke patients and identifying the determinants of stroke severity.
Methods:
A descriptive study was conducted among stroke patients admitted in Govt. Medical College Thiruvananthapuram from August to September 2013. The risk factor profile was studied. A case control comparison was done to identify the determinants of severity of stroke.
Results:
The age of incidence of stroke ranged from 37 years to 88 years. Mean age was 65.30 (SD =12.80). Hypertension was identified as the most common risk factor followed by diabetes, low physical activity and heart diseases. Limb weakness was the most common clinical presentation. Diabetes Mellitus emerged as an independent risk factor of severity with adjusted odds ratio of 3.82 (1.034-14.09).
Conclusion:
Hypertension was the most important risk factor prevalent in stroke patients. Diabetes Mellitus was identified as the only independent determinant of severity of stroke. Early identification of risk factors and its proper management should be done with more rigor, in order to decrease the incidence of stroke and reducing its severity.
Keywords
Risk factors
Stroke
Severity
Thiruvananthapuram
Introduction
Stroke is a global health problem and a leading cause of adult disability.[1] Of 35 million deaths attributable to chronic non-communicable diseases that occurred worldwide in 2005, stroke was responsible for 5.7 million (16.6%) deaths, and 87% of these deaths occurred in low and middle- income counties.[2] It is the second major cause of death worldwide and the fourth major cause of death in India, the death rate being 0.6/1000 in India.[2,3] Kerala is becoming the hotspot of lifestyle diseases and the annual incidence rate of stroke is 1.8/1000. Almost 90% of the cases reported in Kerala are associated with one or two modifiable risk factor(s) in the form of lifestyle diseases.[4] Here lies the importance of a descriptive study, which aims in risk factor profiling, as the early identification and prevention of these risk factors can control the incidence of stroke.
Many of the associated factors and co-morbidities like hypertension, diabetes etc, which are also the known risk factors for stroke, though not completely curable, are treatable and/or modifiable. That is, proper management of these factors plays a major role in stroke prevention as well as limitation of its severity. So this study also tried to find the determinants of severity of stroke with special emphasis on compliance to treatment among the subgroup of patients with known co-morbidities of diabetes and hypertension. This will enable the development of well- planned strategies to manage the same.
Moreover, there had been relatively few studies after acute stroke in Kerala's socio economic set up, that too encapsulating the mentioned apparently relevant dimensions of stroke – Risk factor profile and determinants of severity. Hence this study attains significance from its precisely defined-attainable objectives.
Materials and methods
A descriptive study of risk factor profile of stroke patients along with case control comparisons to find the determinants of severity of stroke was conducted in the Department of Medicine, Govt. Medical College Hospital, Thiruvananthapuram. Patients above 15 years with a definite diagnosis of stroke, admitted in the medical wards during August-September 2013 were selected as the study population. Sample size was calculated using the formula equation 4pq/d[2], where p is the prevalence of hypertension among stroke patients. Here p was taken as 75.8,[5] q is (100-p), d is precision, d was taken as 9%. The minimum sample size that was required was calculated as 90. Accounting for a 10% non-response, the final sample size required was estimated as 100.
Information regarding the relevant variables in the study was collected from the patients admitted to the medical wards, their bystanders and case sheets with the help of a structured questionnaire. Non modifiable risk factors like age, gender and genetic predisposition and the common modifiable risk factors like hypertension, diabetes mellitus, smoking, dyslipidemia, alcohol, obesity, CAD, TIA, lack of exercise were enquired into.[6] As per the WHO STEPS guidelines to measure the prevalence of smoking habit among the respondents, the smokers are categorized as current smokers, current daily smokers, past daily smokers and those who have never smoked in lifetime are classified as non-smokers. Compliance/medication adherence is generally defined as “the extent to which patients take medications as prescribed by their health care providers.”[7] Non-compliant also refers to the one who doesn't monitor and review in time. In our study it was determined by taking into account the % of drugs consumed per week, frequency of disease monitoring and getting medical consultation. Severity of stroke was assessed by National Institutes of Health Stroke Scale (NIHSS) scoring. The NIHSS is one of the most reliable and valid instruments of clinical measurement in stroke.[8] Moreover, NIHSS can be rapidly performed in an acute stroke setting during bedside neurological examination.[9] Accordingly severity was classified into 5 grades; severe, moderately severe, moderate, minor and no stroke symptoms. However for identifying the risk factors of severity, severe and moderately severe categories were grouped as severe stroke and moderate, minor and no stroke symptoms were grouped as non-severe.
Data obtained in the study was subjected to statistical analysis with Statistical Package for Social Sciences (SPSS). The risk factor profiles of stroke patients are expressed as percentage with 95% confidence intervals. Bivariable analysis was done to find the risk factors of severity of stroke using chi- square test. Multivariable analysis was done using logistic regression.
Results
During the 2-months study period, 100 stroke patients were identified. CT scan brain reports were available, according to which stroke could be categorized and it was found that ischemic strokes (71%) greatly outnumbered the hemorrhagic ones (29%).
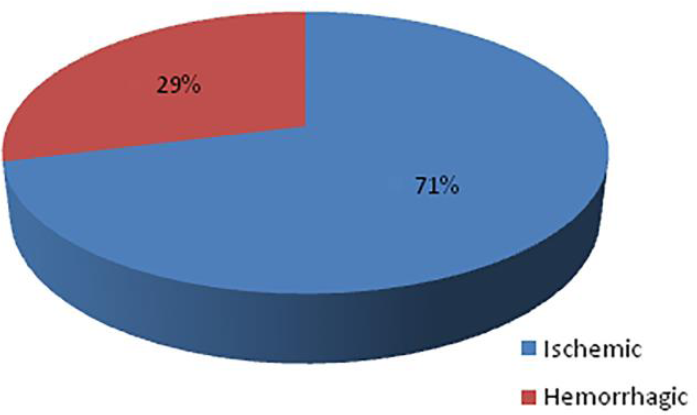
- Types of strokes
The age of incidence ranged from 37 years to 88 years having a mean age of 65.30±12.80. The incidence of stroke was highest in the age group 61-70 years (29%) and least in <50 years (15%). It was slightly more common in males than females (55% against 45%).
Percentage of respondents who were either illiterate or with primary education only was higher compared to the other educational categories. Among the stroke patients studied, 51% were unemployed and 29% were unskilled laborers, the rest being sedentary workers.
Among the stroke patients, 83% (95% CI- 75.63-90.36) had hypertension. Hypertension was more common in females (84.4%) than in males (81.8%) with stroke. Of those diagnosed for hypertension, only 18% were taking the prescribed medicines and following the medical advices correctly, under the guidance of a consultant. The percentage of stroke cases with diabetes mellitus was 49% (95% CI=39.20-58.79). In patients with stroke, 51.1% of females and 47.3% of males were having diabetes mellitus. The total mean time spent (in minutes) in doing physical activity at work, while traveling for work and recreation was estimated to be 4.9hrs.
17% patients with stroke had evidence of coronary artery disease. Rheumatic heart disease was seen only in 4% of the study subjects. 6% had valvular heart disease and 10% had atrial fibrillation.
Of the total stroke patients, 25% (95% CI=16.51-33.48) were smokers, none of whom were females. This was a little high compared to alcoholism (21%) and pan chewing (16%) which also showed similar male-female trends.
Figure 3 presents the percentage of respondents, in various categories of smokers. The prevalence of smoking increased with age till the age group of 50 to 60 years after which it stagnates. The mean age of initiation of cigarette smoking was estimated to be 21.4 years. Males were more among daily smokeless tobacco users (56.3%). The mean age of initiation of smokeless tobacco use was 28.95 years. The proportion of respondents who consumed alcohol regularly was 21% and all were males. 12% respondents were past drinkers. The mean age of initiation of alcohol among the stroke patients under study was 24.38 years.
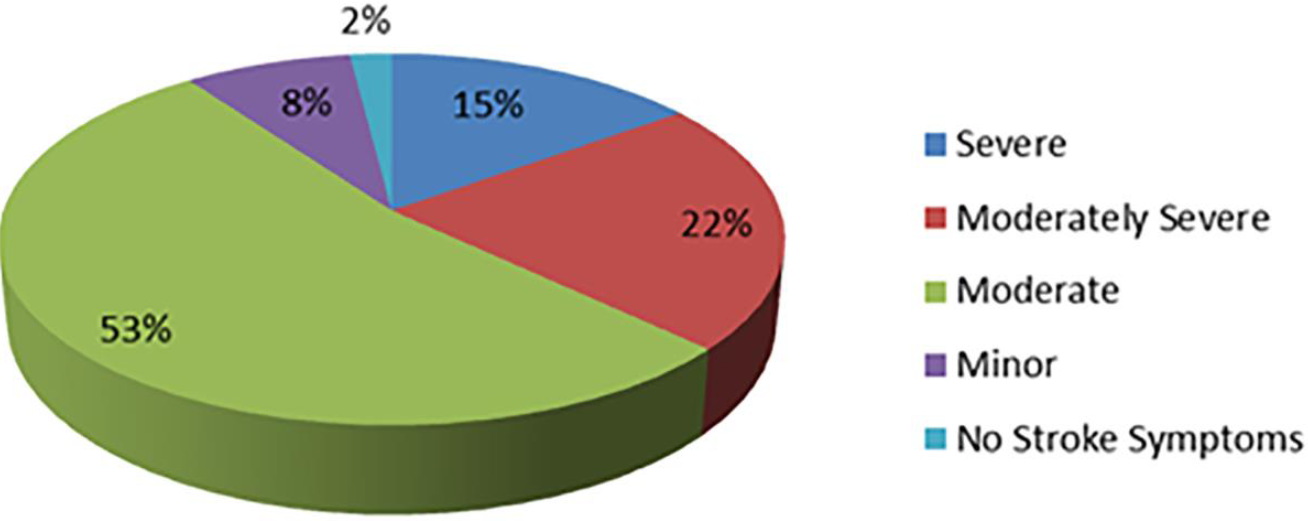
- Pie chart showing the grades of severity of strokes assessed by NIH scale

- Frequency of smoking, pan chewing and alcoholism
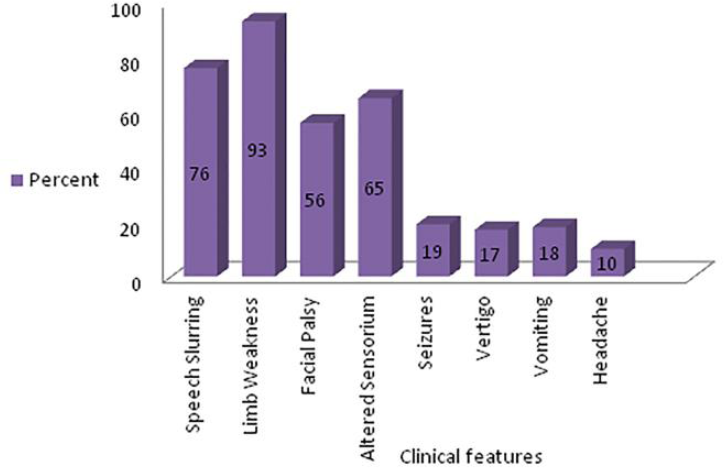
- Different clinical features at the time of presentation
The pattern and clinical features of severe stroke when compared to non-severe stroke is given in Table 1
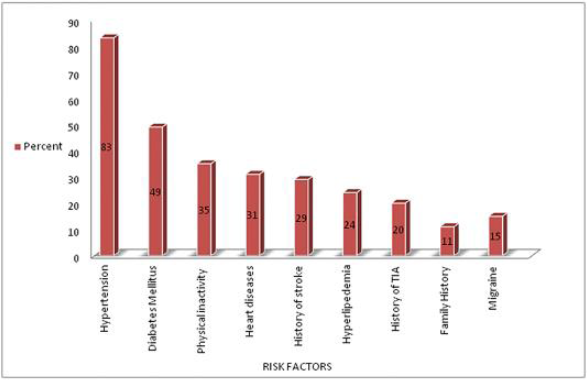
- Risk factors of stroke
| Variable | Category | severe stroke (n=37) No (%) |
Non-severe stroke (n=63) No (%) |
p | Odds Ratio (95% CI) |
|---|---|---|---|---|---|
| Type of Stroke | Ischemic | 20(54.1%) | 51(81%) | 0.004 | 0.28(0.112-0.68) |
| Hemorrhagic | 17(45.9%) | 12(19%) | |||
| Clinical Features | Speech slurring | 27(73%) | 49(77.8%) | 0.587 | 0.77(0.3-1.9) |
| Limb weakness | 37(100%) | 56(88.9%) | 0.03 | ||
| Facial palsy | 27(73%) | 29(46.0%) | 0.009 | 3.16(1.31-7.6) | |
| Altered sensorium | 33(89.2%) | 32(50.8%) | 0.000 | 7.9(2.5-25.2) | |
| Seizures | 10(27.0%) | 9(14.3%) | 0.12 | 2.2(0.8-6.1) | |
| Vertigo | 2(5.4%) | 15(23.8%) | 0.018 | 0.18(0.03-0.8) | |
| Vomiting | 6(16.2%) | 12(19.0%) | 0.72 | 0.82(0.28-2.4) | |
| Headache | 5(13.5%) | 5(7.9%) | 0.37 | 1.8(0.48-6.73) |
Figure 2 shows the frequency of different risk factors in the population studied. Severity was highest in the age group 61-70 years. Stroke in females was found to be more severe (54%) but not statistically significant. It was found that in patients who were either illiterate or with primary education only, severity was significantly higher (86.5%) (chi square-0.002). Non-compliance to treatment of co-morbidities was higher in those with severe stroke, although it was not statistically significant (Table 2).
| Variable | Category | Severe stroke (n=37) No (%) |
Non severe stroke(n=63) No (%) |
p | Odds Ratio (95% CI) |
|---|---|---|---|---|---|
| Diabetes Mellitus | Non-compliant | 15(88.2%) | 17(73.9%) | 0.263 | 2.64(0.46-15.1) |
| Hypertension | Non-compliant | 17(89.5%) | 29(69.0%) | 0.08 | 3.81(0.77-18.9) |
18.3% of diabetic and 26.5% of hypertensives were identified only on hospitalization after stroke. Hence they were not under treatment of these co-morbidities. Table 3 shows the relation between risk factors of stroke and severity. After multivariable analysis, Diabetes Mellitus emerged as an independent risk factor of severity with adjusted odds ratio of 3.82 (1.034-14.09).
| Risk factor | Severe stroke (n=37) | Non-severe stroke (n=63) | p | Odds Ratio (95% CI) |
|---|---|---|---|---|
| Hypertension | 81.1% | 84.1% | 0.695 | 0.809(0.28-2.3) |
| Diabetes Mellitus | 64.9% | 39.7% | 0.015 | 2.8(1.2-6.5) |
| Smoking | 16.2% | 30.2% | 0.120 | 0.45(0.16-1.25) |
| Alcohol | 21.6% | 20.6% | 0.91 | 1.06(0.39-2.8) |
| Hyperlipidemia | 29.7% | 20.6% | 0.304 | 1.62(0.64-4.13) |
| Heart disease | 18.9% | 38.1% | 0.04 | 0.38(0.14-0.99) |
Discussion
This study was hospital-based. Patients were identified using an internationally recognized definition of stroke. The age of incidence ranged from 37 to 88 years with the mean age of stroke being 65.30±12.80 years. This was almost similar to the findings of a study from Central Kerala where the age of incidence ranged from 28 years to 84 years with a mean age of 63 (standard deviation 13.01).[10] The mean age was 64.78±9.40 years, range 45–85 in a prospective hospital based study.[5] The mean age was 62.20 in a study done in Malaysia.[11] The present study stands in support for the same fact previously mentioned by Framingham study and a study from Central Kerala because majority of the patients were above 50 years.[10,12]
In this study, 55% were males and 45% were females. There were 57.7% men and 47.3% women in a hospital based study done in Kashmir,[5] where the age group studied was 45 to 85 years. 48.2% were male and 51.8% were females in a study from Malaysia.[11] The risk of incidence of stroke increases with age.[13] However, the increase in number of males among stroke patients was not statistically significant.
It was found in this study that the mean age group for females was more than that for males. This is similar to that reported by Trivandrum stroke registry.[4] So the inference is that males may get stroke much earlier than females. This may be due to the protective effect of estrogen in females till menopause.
The frequencies of ischemic and hemorrhagic stroke were 71% and 29% respectively. The frequencies of Ischemic and hemorrhagic stroke in Trivandrum Stroke Registry was 83.6% and 16.4% respectively.[4] In another study also,[10] ischemic strokes greatly outnumber the hemorrhagic strokes (84.7 % versus 15.3 %), all standing for the fact mentioned by K. Park.[3]
Regarding the presentations of stroke, the most common was weakness constituting 93%. Following weakness, the second most common manifestation found was speech slurring followed by altered sensorium and facial palsy. Seizures & vertigo were less common. This is a due support to the work done by in the neuro-epidemiologic study.[14] Among weakness the most common presentation seen was hemiplegia or hemiparesis, that substantiates the central Kerala study.[10] The major (modifiable) behavioral risk factors identified in the World Health Report 2002 are tobacco use, harmful alcohol use, unhealthy diet (low fruit and vegetable consumption) and physical inactivity. On the other hand, the major biological risk factors identified are overweight and obesity, raised blood pressure, raised blood glucose and raised total cholesterol. These major behavioral and biological risk factors were included in the risk factor profile study except diet and overweight since most of the patients were bed ridden and therefore the anthropometric measurements could not be taken. In addition, the survey questionnaire asked questions about certain life style of respondents which could be considered as the behavioral risk factors for stroke. They included tobacco smoking and chewing, alcohol consumption, and physical activity among men and women aged >15 years.
Hypertension was the most common risk factor (83%) of cerebrovascular accident in the study which was closer to the results of another study (75.8%).[5] In other studies, the proportion of hypertensives among stroke patients were much lesser, that is, about 46% and 40%.[6,10,15] Studies reported hypertension as the most common risk factor in 63% of Iranian women and only in 42% of men with ischemic stroke.[16] In our study also, hypertension was more common in females (84.4%) than in males (81.8%) with stroke.
Diabetes mellitus is an important marker of risk for stroke. In the study, the history pertaining to diabetes was elicited from the respondents. It is found that a good correlation exists between diabetes and stroke. 49% of the study population had reported raised blood glucose, which is almost similar to the value proposed in another study, whereas it was 6% in the general population of Kerala from the data of Integrated Disease Surveillance Project (IDSP).[16,17] The frequency of diabetes was 12% in a randomized controlled study and it was 16.1% in a study from Kashmir.[5,15] Thus the finding is much higher than found in other studies. An epidemiologic study from China on stroke patients showed that female patients were having higher of prevalence of diabetes mellitus.[18] In the present study, patients with stroke, 51.1% of females and 47.3 % of males were having diabetes mellitus. The compliance to treatment was elicited from the diabetic subjects and it was found that only 16.3% were compliant.
Smoking is an established risk factor of stroke.[19] In this study, it was found that 25% were smokers which are similar to the results of Central Kerala study,[10] and slightly lower than the 31% value obtained in another study.[6] In the present study all the smokers were males. But in another study from USA,[20] 30.4% females from the cohort had a past history of smoking as compared to 61.7% males (odds 0.27, 95%CI 0.16 to 0.46; P< 0.0001). Among the addictions taken into consideration (smoking, alcoholism & pan chewing), the most common risk factor found was smoking which supports the findings of another study.[6] The percentage of current smokeless tobacco user was 16% which is higher than the prevalence of pan chewing among general population of Kerala (5%) as per IDSP results.[17]
Low physical activity leads to obesity, dyslipidemia (lower high-density lipoprotein levels), insulin resistance, diabetes mellitus and high blood pressure level. Low physical activity as such is therefore a well-established risk factor for cerebrovascular accident as in most of the other non- communicable diseases. In this study, 35% were with low physical activity.
Prevalence of CAD among stroke [17%] has not reached the value proposed by another study (44.9%).[5] The reason for such a big difference may be the large difference between the life style patterns of our society and others, poor socioeconomic status and also better awareness regarding the dietary pattern. It can also be due to the good compliance to the prescribed diet after having an attack of ischemic heart disease. However, in a study from Central Kerala,[10] the frequency of CAD was only 3%. In the present study atrial fibrillation was found in 10% stroke patients which is almost similar to the result (17%) from a randomized control trial and a study from Kashmir (12%).[5] In another study, females had 0.51 times odds for having coronary artery disease (P = 0.024) as compared to males.[15,20]
Hyperlipidemia along with long term diabetes, hypertension and smoking are the risk factors for developing atherosclerosis, which is a possible cause of ischemic stroke. In our study, hyperlipidemia was present in 24% stroke patients as against the 69.8% in another study.[5]
In this study, history of Transient ischemic attack (TIA) was present in 20% and history of prior stroke in 29% against 17% and 19% respectively in another study.[15] This proves the necessity of the early detection and management of stroke and TIA to prevent any consequent stroke. But in a study from Central Kerala,[10] history of TIA was present only in 8.8%.
The stroke risk profile provides the framework for identification of those individuals at sufficiently increased risk of stroke to warrant vigorous risk factor management. From this study hypertension, diabetes mellitus, low physical activity and heart diseases were identified as the common risk factors. The study from Thiruvananthapuram, Kerala,[6] regarding the risk factors of cerebral infarction also stands in line to this.
Initial severity of stroke, often measured by the NIHSS score, has been shown to be a powerful predictor of mortality and functional outcome after stroke in many studies.[21-23] In this study, only 2% were with no stroke symptoms. There were 22% moderately severe and 15% severe patients. Majority came under moderate grade of severity (53%). In a study from Kashmir, only 1.3% were of no symptoms. Moderately severe and severe grades constituted 34.9% each. Slight and moderate grade constituted only 12.1%. This difference may be due to the availability of better health care facilities here or due to the difference in the scales used to assess the severity.
Stroke in females was found to be more severe (54.1%). But in another study, there was no difference in the stroke severity on arrival as defined by NIHSS between females and males. The present study suggested that limb weakness, altered sensorium, facial palsy at the time of presentation were significantly higher in severe stroke. A significant association of diabetes mellitus with severity (p=0.015 OR=2.8(1.2-6.5)) was also noticed. But in another study, no significant correlation between blood sugar and severity was observed, while the stroke severity was significantly correlated with the blood cholesterol and triglyceride levels only.[24] Nevertheless, controversial results are observed in the findings of other studies, for instance, the stroke patients with high levels of blood sugar at the time of hospitalization were at a higher risk of death within the first 30 days.[25] Another research also mentioned that hyperglycemia can cause a higher rate of mortality and a lower ability of functional recovery.[26]
Delay in receiving treatment and non-compliance to treatment of co-morbidities also were associated with increased severity. Only 16.3% of diabetic patients in the present study were adherent to the treatment. It was found that, 88.2% of the severe patients were not compliant to the treatment of diabetes. In a study done among elderly in an urban slum of Delhi,[27] only one-third of the diabetic participants were aware of their condition; two-thirds of these were on treatment and three-fourths of those on treatment had controlled fasting blood sugar level. Another study came up with the results that only 10% of people with type 2 diabetes have an endocrinology visit.[28] Similarly, only 18% of hypertensives in the study done were compliant to its treatment. 89.5% of the severe patients were not compliant to the treatment of hypertension. In a study, only 20% of the study population was on treatment and only 6.6% had blood pressure control.[29] A key factor contributing to poor blood pressure control is suboptimal adherence to prescribed therapy. Despite numerous studies conducted over the last 50 years to identify the best method for increasing patient compliance, no single intervention has emerged as superior to the others.[30] All these studies support the derived findings of the present study. Immediate measures are to be taken to solve this problem as diabetes and hypertension are the important risk factors of stroke as well as its severity.
References
- Preventing stroke: saving lives around the world. Lancet Neurol. 2007;6:182-7.
- [CrossRef] [PubMed] [Google Scholar]
- Park's Textbook of Preventive and Social Medicine. (22th). Jabalpur: Bhanot; 2013. p. :348-349.
- [CrossRef] [Google Scholar]
- Incidence, types, riskfactors and outcome of stroke in developing country-The Trivandrum Stroke Registry. Stroke. 2009;40:1212-1218.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of mortality after acute stroke: A prospective hospital based study. J Ayub Med Coll Abbottabad. 2011;23:144-146.
- [Google Scholar]
- Risk factors for acute ischaemic stroke in young adults in SouthIndia. J Neurol Neurosurg Psychiatry. 2007;78:959-963.
- [CrossRef] [PubMed] [Google Scholar]
- A reappraisal of reliability and validity studies in stroke. Stroke. 1996;27:2331-2336.
- [CrossRef] [PubMed] [Google Scholar]
- Handbook of neurologic rating. (2nd). Newyork: Demos medical publishing; 2006. p. :261-277.
- [CrossRef] [Google Scholar]
- A Study on the Patterns and Risk factors of Stroke in Patients from Central Kerala. Kerala Medical Journal. 2011;11:194-199.
- [Google Scholar]
- Predictors of in-hospital mortality after an acute ischaemic stroke. Neurol J Southeast Asia. 2003;8:5-8.
- [Google Scholar]
- Current Status of Risk Factors of Stroke: The Framingham Study. Neuro Clin. 1983;1:317-43.
- [CrossRef] [PubMed] [Google Scholar]
- Neurological emergencies: Acute Stroke. J. Neurology, Neurosurgery & Psychiatry. 2000;68:277-88.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for ischaemic stroke:a case control analysis. Neuroepidemiology. 1992;11:24-30.
- [CrossRef] [PubMed] [Google Scholar]
- Stroke Units Versus General Medical Wards, I: Twelve and Eighteen-Month Survival, A Randomized, Controlled Trial. Stroke. 1998;29:58-62.
- [CrossRef] [PubMed] [Google Scholar]
- The Khorasan Stroke Registry: Results of a five-year hospital-based study. Cerebrovasc Dis. 2007;23:132-9.
- [CrossRef] [PubMed] [Google Scholar]
- Government of India Ministry of health and family welfare. Available from: http://www.idsp.nic.in/
- [Google Scholar]
- Age and gender specific prevalence of risk factors in patients with first-ever ischemic stroke in China. Stroke Res Treat. 2012;10:51-5.
- [CrossRef] [PubMed] [Google Scholar]
- Cigarrete smoking as a risk factor for stroke: The Framingham Study. JAMA. 1988;259:1025-9.
- [CrossRef] [PubMed] [Google Scholar]
- Female Gender Remains an Independent Risk Factor for Poor Outcome after Acute Non-traumatic Intracerebral Hemorrhage. Neurology Research International 2013 Available from: http://dx.doi.org/10.1155/2013/219097
- [CrossRef] [PubMed] [Google Scholar]
- Baseline NIH Stroke scale score strongly predicts outcome after stroke: a report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST) Neurology. 1999;53:126-31.
- [CrossRef] [PubMed] [Google Scholar]
- A predictive risk model for outcomes of ischemic stroke. Stroke. 2000;31:448-55.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of survival and functional outcome in acute stroke patients admitted to the stroke intensive care unit. Journal of the Neurological Sciences. 2008;270:60-66.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic factors in acute stroke, regarding to stroke severity by Canadian Neurological Stroke Scale: A hospital-based study. Asian J Neurosurg. 2013;8(2):78-82.
- [CrossRef] [PubMed] [Google Scholar]
- Another reason to avoid a sugar high: Study links high blood sugar to mortality after stroke. Stroke. 2003;69:842-56.
- [Google Scholar]
- Stress hyperglycemia and prognosis of stroke in Nondiabetic and diabetic patients. Stroke. 2001;32:24-6.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence, awareness, treatment and control of diabetes among elderly persons in an urban slum of Delhi. Indian J Community Med. 2012;37:236-9.
- [CrossRef] [PubMed] [Google Scholar]
- Type 2 diabetes in France: epidemiology, trends of medical care, social and economic burden. Presse Med. 2013;42:830-8.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence, awareness, treatment, control and risk factors for hypertension in a rural population in South India. Int J Public Health. 2012;57:87-94.
- [CrossRef] [PubMed] [Google Scholar]
- Methods to improve medication adherence in patients with hypertension: current status and future directions. Curr Opin Cardiol. 2005;20:296-300.
- [CrossRef] [PubMed] [Google Scholar]






