Translate this page into:
Prevalence of Serum Vitamin D Deficiency and Insufficiency in Cancer
*Corresponding author: Samarpita Koner, Department of Food and Nutrition, Swami Vivekananda University, Kolkata, West Bengal, India. samarpitakoner.2104@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shaw J, Koner S, Roy Choudhury S, Singh K, Ghosh J. Prevalence of Serum Vitamin D Deficiency and Insufficiency in Cancer. J Compr Health. 2024;12:75-82. doi: 10.25259/JCH_7_2024
Abstract
Fat-soluble Vitamin D plays a critical role in maintaining bone health and regulating the absorption of calcium and phosphorus. Interest in Vitamin D’s potential role in treating and counteracting malignant development has grown recently. According to epidemiological research, higher Vitamin D levels may be associated with a lower risk of developing certain cancers, such as colorectal, breast, and prostate cancer. The current investigation aims to determine the correlation between the prevalence of Vitamin D deficiency in the serum and the development of cancer. Studies conducted in research centers have also suggested that Vitamin D may possess anti-malignant growth characteristics, such as the ability to trigger apoptosis (a modified form of cell death) and inhibit the proliferation of malignant development cells. However, the results of the first clinical trials investigating the use of Vitamin D as a preventative or malignant growth therapy have been mixed, and the optimal dosage and duration of Vitamin D supplementation for illness prevention or treatment remain unclear. Additional research is anticipated to identify subpopulations that may benefit most from Vitamin D supplementation and to clarify the potential benefits and risks of this medication for malignant growth anticipation. Nevertheless, ensuring adequate Vitamin D intake through supplementation or sun exposure may be a key strategy for reducing the risk of cancerous development and improving overall health.
Keywords
Cancer
Vitamin D
Vitamin D supplements
Diet
Malignant growth
INTRODUCTION
When people spend more time indoors at work or home, they do not get enough sunlight to produce enough cutaneous Vitamin D.1-3 Consequently, Vitamin D deficiency has become a significant health risk in the modern era. Recent studies conducted worldwide have consistently demonstrated that Vitamin D deficiency is unexpectedly prevalent across all age groups.3 Worldwide, between 30% and 50% of the population lacks enough vitamin D.4 In community-based Indian studies conducted over the past decade on seemingly healthy controls, the prevalence varied between 50% and 94%.5 Vitamin D, a fat-soluble steroid hormone, has been extensively studied for its ability to balance calcium and phosphorus levels, thereby supporting strong bones. Beyond just maintaining bone health, its importance extends to immune regulation, heart health, mineral metabolism, and bone remodeling.6 The serum 25(OH)D test was used to assess the Vitamin D level in individuals diagnosed with multiple myeloma.7 An earlier study determined that a cutoff value of ≥30 ng/mL was appropriate for this application. Vitamin D insufficiency and deficiency are frequently associated with worse overall survival (OS) and relapse-free survival in hematological malignancies and diseases, higher malignant cell burden, poor response to treatment, and worse health outcomes.7 Higher apoptosis, reduced angiogenesis, and higher cell cycle arrest lead to a slower rate of proliferation.8 An increased risk of bone fracture and early signs of altered bone microarchitecture are common characteristics of monoclonal gammopathy of undetermined significance (MGUS), a pre-malignant condition. Because Vitamin D is essential for the metabolism of minerals and bone, its deficiency is associated with the development of metabolic bone illnesses such as rickets and osteomalacia.9 Recent research has connected the non-skeletal effects of Vitamin D to a variety of ailments, including infections, diabetes mellitus, autoimmune diseases, and cardiovascular diseases.10 Numerous epidemiological studies have found a connection between Vitamin D deficiency and cancer. Higher levels of Vitamin D have been associated with decreased mortality from liver, colon, and breast cancers.11
Moreover, Vitamin D from diet and sun exposure has been associated with a decreased risk of cancer.12 There are not many studies that examine how common Vitamin D deficiency is among cancer survivors. In a 2007 study conducted in the United States (US), 76 out of 99 breast cancer survivors (77%) and 51 out of 54 controls (94%) showed Vitamin D deficiency (<32 ng/mL).13 In a unique multiethnic cohort study carried out in the US, the mean Vitamin D level was 24.8 ± 10.4 ng/mL, and 75.6% of the 790 breast cancer survivors had low serum 25(OH) D.14 In a second study, 29% of the patients had insufficient levels of 25(OH)D (below 20 ng/mL), and the mean Vitamin D level was found to be 25.2 ± 10.37 ng/mL among a large and diverse group of cancer survivors in a pediatric cancer survivor clinic.15 The current investigation aims to determine the correlation between the prevalence of Vitamin D deficiency in the serum and insufficiency in cancer.
WHAT IS CANCER?
The word “disease” refers to a broad category of conditions characterized by the unchecked growth and dissemination of abnormal cells within the body. These cells have the ability to invade and destroy healthy tissues, engulf tumors, and metastasize – or spread – to other parts of the body through the lymphatic or circulatory networks. There are many different types of diseases, such as leukemia, prostate disease, breast cancerous growth, colon cancerous growth, and cellular disintegration in the lungs.16 Every type of cancerous tumor has unique characteristics and options for care. Many factors can contribute to disease, such as genetic changes, exposure to certain natural elements (e.g., radiation, tobacco smoke, and synthetic substances), and lifestyle choices (e.g., poor eating habits, inactivity, and excessive alcohol consumption).17 For the purpose of addressing the illness and enhancing endurance potential, early diagnosis and treatment are crucial.
EPIGENETIC FACTORS RESPONSIBLE FOR CANCER
Malignant growth is a perplexing illness that can be brought about by different elements, including hereditary and epigenetic changes.18 Epigenetic changes allude to adjustments to DNA that do not change the fundamental hereditary code yet can, in any case, influence quality articulation and cell capability.18 There are a few epigenetic factors that have been ensnared in the improvement of disease, including:
DNA methylation
This is a cycle wherein a methyl bunch is added to the DNA particle, which can prompt quality hushing. Variant DNA methylation designs have been related to a few sorts of malignant growth.19
Histone changes
Histones are proteins that assist with bundling DNA into a reduced construction called chromatin. Changes to histones, such as acetylation, methylation, and phosphorylation, can influence how firmly DNA is bundled and thusly impact quality articulation. Dysregulation of histone adjustments has been connected to the advancement of disease.20
Non-coding RNAs
Non-coding RNAs are RNA particles that do not encode proteins yet, at the same time, assume a part in directing quality articulation. Strange articulation of certain non-coding RNAs has been seen in malignant growth cells.21
Chromatin rebuilding
This alludes to changes in the design of chromatin that can influence quality articulation. Adjustments in chromatin rebuilding factors have been related to the improvement of disease [Figure 1].22
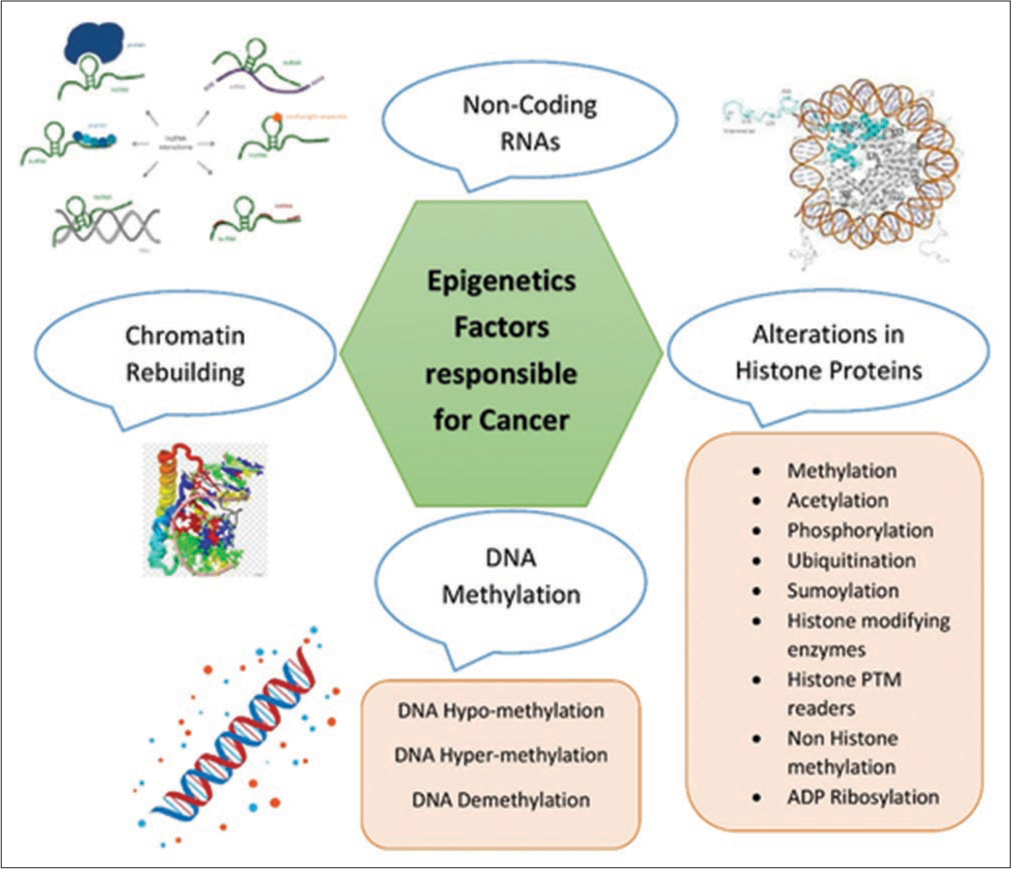
- Epigenetic factors responsible for cancer.
Ecological variables
Natural elements, such as openness to poisons or stress, can likewise prompt epigenetic changes that add to disease advancement.23
By and large, epigenetic modifications can add to the inception, movement, and metastasis of disease. Understanding the fundamental systems of these progressions might help in the improvement of novel treatments for malignant growth treatment.24
WHAT IS VITAMIN D?
One important supplement that assumes some basic functions in the body is Vitamin D. Its primary function is to facilitate the body’s absorption and utilization of calcium and phosphorus, two elements necessary for healthy bones and teeth. Ghosh et al., 2020 and 2021. In addition, Vitamin D regulates the immune system, maintains cardiovascular health, and may help prevent some types of cancerous growth.2,25 Deficit in Vitamin D can lead to a number of health problems, such as osteoporosis, weakness in the muscles, and an increased risk of fractures and falls. Serious Vitamin D deficiency in children can result in rickets, a disorder that causes twisted and fragile bones.1 The best source of Vitamin D is sunshine, which causes the skin to produce Vitamin D on its own. However, a lot of people do not receive enough sun exposure to meet their Vitamin D needs, especially in areas with limited daylight or during the winter months. Furthermore, certain individuals may be more susceptible to Vitamin D deficiency due to factors such as age, skin tone, and dietary habits. Young and Xiong et al. (2018), to ensure adequate levels of Vitamin D, some people may need to take supplements or consume foods high in Vitamin D, such as fatty fish, egg yolks, and fortified dairy products.11 Speaking with a medical care provider regarding the appropriate dosage and source of Vitamin D based on personal needs and health state is very important.26
HOW DOES VITAMIN D WORK AGAINST CANCER?
In addition to playing a key role in maintaining bone health, Vitamin D is a fat-soluble substance that has been shown to have anti-cancer growth capabilities.27 Although the precise mechanism by which Vitamin D inhibits cancerous growth is not fully understood, it is believed to involve a few distinct pathways.28 One way that Vitamin D counteracts illness is through controlling the division and growth of cells. Vitamin D accelerates cell separation and reduces cell multiplication, which can impede the growth of malignant growth cells. This suggests that disease-causing cells are less likely to divide and grow out of control, which may lead to the organization of growth.18
Another way that Vitamin D inhibits cancerous growth is by promoting apoptosis, or the altered death of cells. Malignant growth cells can be triggered by Vitamin D to undergo apoptosis, which helps to stop the spread of these cells throughout the body. In addition, Vitamin D can help reduce irritation, which is a major factor in the improvement of malignant growth. Reducing annoyance may help prevent the progression of illness since chronic irritation can promote the growth and spread of cancerous growth cells.29 In general, research suggests that Vitamin D may help regulate cell development and division, promote apoptosis, and lessen aggravation, all of which may help prevent the turn of events and spread of malignant growth, even though the precise mechanisms by which it neutralizes disease are not fully understood.30
MECHANISM OF ACTION
Supplementing with Vitamin D is important since it plays a major role in many physiological cycles in the body, such as bone health, the formation of the immune system, and cell division and growth.31 More and more evidence is mounting that suggests Vitamin D may have anti-malignant growth capabilities. Although the exact mechanisms by which Vitamin D could inhibit cancerous growth are not fully understood, research suggests that it could function in multiple ways:
Cell multiplication hindrance
It has been demonstrated that Vitamin D inhibits the growth and division of cancerous growth cells both in vitro and in vivo. It may accomplish this by impeding the function of particular proteins involved in cell division and development.32
Acceptance of apoptosis
It has been shown that in malignant development cells, Vitamin D triggers apoptosis, also known as tailored cell passing. This could occur through the activation of signaling that results in cell passage.33 Cell separation guidelines: Vitamin D may play a role in controlling the differentiation of cancerous progenitor cells into non-cancerous ones. This could be a result of the relationship between Vitamin D and the division of normal cells.34
Angiogenesis inhibition
According to Chen and Zhu, Vitamin D may inhibit the formation of new blood vessels that malignancies require to grow and spread.35
Balance of safe capability
Research on Vitamin D’s regulation of resistant capability suggests that it may have some anti-malignant growth capabilities. It may enhance the migration of susceptible cells that attack cancerous cells while inhibiting the activity of resistant cells that promote the growth of cancer.36
Mitigating effects
Vitamin D has soothing effects that may be helpful in treating or preventing certain types of cancerous development. Chronic annoyance is a risk factor for certain diseases.37
Research is currently being done to determine the precise mechanisms through which Vitamin D inhibits malignant development. However, the evidence suggests that it may function through a variety of routes to prevent the growth and dissemination of disease cells.37
VITAMIN D STATUS IN RELATION TO BREAST CANCER
There is evidence to suggest that low Vitamin D levels may be associated with an increased risk of developing a cancerous tumor in the bosom. In addition to being important for maintaining healthy bones and safe function, Vitamin D also plays a role in regulating cell division and development, two processes that can have detrimental effects on the development of cancer.38 According to several studies, women who have higher blood levels of Vitamin D are less likely to develop breast cancer than those who have lower amounts. However, the precise relationship between Vitamin D and bosom malignant growth is still being considered, and more research is anticipated to understand the relationship fully.39 It is important to remember that, even though there is evidence to suggest that Vitamin D may help counteract breast malignant growth, taking Vitamin D supplements is not a replacement for other screening and prevention measures for breast diseases, such as mammograms and healthy lifestyle choices such as maintaining a healthy weight, exercising frequently, and refraining from smoking and excessive alcohol consumption. It is a good idea to discuss any concerns you may have with your healthcare provider, such as your Vitamin D levels or your risk of bosom malignant growth.40
VITAMIN D STATUS IN RELATION TO COLON CANCER
A growing body of research indicates that there may be a link between colon cancerous development and Vitamin D deficiency.41 Supplementing with Vitamin D is essential for maintaining regions of strength, but it also has a role in controlling cell division and development, resistance, and reducing inflammation – events that may contribute to the advancement of colon cancerous growth. Certain tests have indicated that individuals with low blood levels of Vitamin D are more likely to develop colon cancer.42 According to a large meta-analysis of observational studies, people with the highest levels of Vitamin D compared to those with the lowest had a 30% decreased risk of developing colon cancerous development.43 However, further research is needed to fully understand the relationship between Vitamin D levels and colon cancerous progression.44 It is anticipated that randomized controlled preliminary studies will determine the best times and dosages for Vitamin D administration, as well as if it can assist in preventing or treating colon cancerous development. It is important to remember that maintaining adequate Vitamin D levels is important for overall health, but it is not a replacement for other recommended malignant growth prevention strategies, such as routine screening, maintaining a healthy weight, abstaining from tobacco, and limiting excessive alcohol consumption.45
VITAMIN D STATUS IN RELATION TO PROSTATE CANCER
A growing body of research is looking into the relationship between prostate cancer risk and Vitamin D levels.46 A fat-solvent nutrient, Vitamin D plays a key role in maintaining bone health, safe function, and calcium retention. Being resistant to illness is also acknowledged.47 A few observational studies have suggested a possible link between low Vitamin D levels and an increased risk of prostate cancerous development. Men with higher circulating degrees of Vitamin D had a lower risk of developing prostate cancerous growth compared to individuals with lower levels, according to a meta-analysis of 25 studies.48 However, the evidence is not entirely consistent, and some studies have not discovered a strong correlation between Vitamin D levels and the risk of prostate cancer growth. Furthermore, it is still unclear what level of Vitamin D is optimal for preventing prostate cancerous growth, and it is unknown if raising Vitamin D levels may prevent or cure prostate disease. Overall, research is anticipated to clarify the association between higher Vitamin D levels and prostate cancer risk, even if there is evidence to support that such levels may be protective against cancerous growth.49
VITAMIN D STATUS IN RELATION TO SKIN CANCER
It is confusing and still not fully understood how skin malignant development and Vitamin D levels are related.50 According to certain tests, individuals with greater Vitamin D levels may be less likely to promote some types of skin cancer, such as melanoma. Vitamin D is produced in the skin when the skin is exposed to bright (ultraviolet [UV]) radiation from daylight.51 However, it is also well-established that excessive UV exposure is the primary cause of skin disease and that avoiding unwarranted sun exposure and wearing protective clothing and sunscreen can significantly reduce the risk of developing skin cancer. Furthermore, even though Vitamin D has many important health benefits, taking supplements or extra Vitamin D can lead to adverse health effects like hypercalcemia, which is an increase in blood calcium levels.52 To reduce the risk of skin cancer development and to maintain adequate Vitamin D levels, it is imperative to maintain a balance between Vitamin D intake and sun protection.53
TRIALS GOING ON VITAMIN D WITH RELATION TO DIFFERENT CANCER THERAPY
Growing evidence suggests that Vitamin D may be important in the therapy of malignant development.54 Here are a few examples of research that examined the effects of Vitamin D when combined with different treatments for malignant growths:
Bosom malignant growth
In women with metastatic bosom malignant growth receiving aromatase inhibitor treatment, high-portion Vitamin D supplementation (4000 IU/day) further developed movement-free endurance, according to a 2018 randomized controlled preliminary published in JAMA Oncology.11
Advanced prostate cancer
A 2015 review published in the Journal of Clinical Oncology revealed that men with advanced prostate cancer who received a high portion of Vitamin D supplementation (10,000 IU/day) in addition to standard treatment had a longer median survival time than those who received standard treatment alone.55
Colorectal malignant growth
Vitamin D administration may improve overall endurance in patients with colorectal malignant growth, according to a comprehensive survey and meta-analysis published in the Diary of Clinical Oncology in 2019.
Melanoma
According to 2016 research published in the Journal of Clinical Oncology, individuals with metastatic melanoma who received high-portion Vitamin D supplementation (up to 20,000 IU/day) in addition to normal treatment showed improved movement-free endurance.56
EPIDEMIOLOGY OF CANCER ALL OVER THE WORLD
The study of illness transmission varies throughout different regions of the world, and malignant growth is a complex infection with many types and random causes. I can provide you with an overview based on the data available until September 2021, even though it is unrealistic to anticipate providing a thorough analysis of the research on disease transmission worldwide.57
Frequency and death rates
Due to differences in population socioeconomics, lifestyle variables, healthcare systems, and access to early detection and therapy, the prevalence and death rates of malignant growth mostly differ between countries and locations.11 Large salary nations will typically have greater incidence rates, primarily due to factors like aging populations and improved malignant growth detail frameworks. Either way, as the population grows, ages, or changes in gambling conditions, disease incidence rates are rising globally.58
Driving kinds of disease
The most known types of cancer in general include stomach, colon, lung, and prostate cancers. However, the area-specific appropriation and relative importance of explicit tumors can vary. For example, cellular degeneration in the lungs is more common in countries with substantial tobacco use, while stomach cancerous development is more common in some regions of Asia. The most well-known illness affecting women worldwide is breast cancer.20
Risk elements
Some risk factors contribute to the progression of the illness: Smoking, poor diet, real inactivity, obesity, infections (e.g., hepatitis B and C and human papillomavirus), alcohol use, exposure to environmental carcinogens, and genetic predisposition. Different populations and regions have different levels of importance and prevalence of these gambling characteristics.11
Local contrasts
Districts may differ in the weight of malignant growth and how it is appropriated. For instance, certain low- and middle-income countries may see an increased prevalence of malignancies linked to irreversible specialists, such as human papillomavirus and liver malignant development (hepatitis B and C). On the other hand, countries with high thriving salaries usually have greater rates of cancerous tumors associated with lifestyle concerns, such as lung and colon disorders.59
Avoidance and control endeavors
Systems for preventing and controlling disease vary from nation to nation and are influenced by the availability of resources, the quality of medical care, and the needs of overall health. Objectives typically include promoting healthy lifestyles, implementing cancer screening programs, expanding access to early diagnosis and treatment, and improving disease research. It is important to remember that the study of illness transmission and malignant growth is a distinct discipline with constant research and knowledge development. It is advised to consult reputable sources such as the World Health Organization, the International Agency for Research on Cancer, public disease libraries, or health divisions for the most extraordinary and region-specific data.60
CONCLUSION
The connection between Vitamin D and malignant growth is a subject of continuous exploration, and keeping in mind that a few examinations have proposed a possible affiliation, the proof is not yet convincing. Vitamin D is a supplement that assumes an urgent part in different physiological cycles, including resistant capability, cell development, and guidelines of irritation. Laboratory and observational investigations have shown that Vitamin D might have against disease properties, for example, repressing cell expansion, advancing cell separation, and lessening angiogenesis (the arrangement of fresh blood vessels that help cancer development). In any case, the outcomes from epidemiological examinations looking at the relationship between Vitamin D levels and malignant growth risk have been conflicting. A few investigations have revealed a diminished gamble of specific tumors, including colorectal, bosom, and prostate malignant growth, among people with higher Vitamin D levels. Then again, different examinations have tracked down no huge affiliation or have yielded clashing outcomes. It is critical to take note of that laying out a causal connection between Vitamin D and malignant growth is trying due to different variables. These incorporate the intricacy of malignant growth advancement, the impact of other jumbling factors (such as way of life, hereditary qualities, and sun openness), and the constraints of study plans (such as review examinations and estimation of Vitamin D levels). While the proof is not yet conclusive, keeping up with sufficient Vitamin D levels is, by and large, viewed as helpful for well-being. Vitamin D can be obtained through openness to daylight, dietary sources (such as greasy fish, braced dairy items, and enhancements), or a mix of both. It is fitting to keep the suggested dietary rules and talk with medical services experts for customized counsel on Vitamin D supplementation. Further, examination, including enormous scope clinical preliminaries, is expected to more readily figure out the connection between Vitamin D and malignant growth and to decide whether there are explicit populaces or malignant growth types that might profit from Vitamin D supplementation.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Antimicrobial Effect of 1, 25 Dihydroxy Vitamin D on Vibrio cholerae and Its Association with Serum 25-Hydroxy Vitamin D Level in Rural Elderly Women: An Experimental Study. J Clin Diagn Res. 2021;15:OC34-7.
- [CrossRef] [Google Scholar]
- Period of Sun Exposure and Vitamin D Status among the Rural Elderly Women of West Bengal, India. Indian J Community Med. 2021;46:285-7.
- [Google Scholar]
- Potential Role of Vitamin D as an Antiviral Agent. Med J Dr DY Patil Univ. 2021;14:3-12.
- [CrossRef] [Google Scholar]
- 100 Years of Vitamin D: Global Differences in Vitamin D Status and Dietary Intake: A Review of the Data. Endocr Connect. 2022;11:e210282.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of Hypertension and Its Risk Factors in Rural Kerala, India: A Community-based Cohort Study. Public Health. 2012;126:25-32.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoimmunology: Evolving Concepts in Bone-immune Interactions in Health and Disease. Nat Rev Immunol. 2019;19:626-42.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of Vitamin D Deficiency on the Clinical Presentation and Prognosis of Patients with Newly Diagnosed Multiple Myeloma. Am J Hematol. 2009;84:397-400.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic Implications of Cell Cycle, Apoptosis, and Angiogenesis Biomarkers in Non-small Cell Lung Cancer: A Review. Clin Cancer Res. 2005;11:3974-86.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D Activities and Metabolic Bone Disease. Clin Chim Acta. 2013;425:148-52.
- [CrossRef] [PubMed] [Google Scholar]
- Cathelicidin LL-37 Level in Presence and Absence of Vitamin D in Cultured Macrophages Isolated from Elderly Women. Malays J Nutr. 2022;28:327-34.
- [CrossRef] [Google Scholar]
- Influence of Vitamin D on Cancer Risk and Treatment: Why the Variability? Trends Cancer Res. 2018;13:43-53.
- [Google Scholar]
- Vitamin D and Sunlight: Strategies for Cancer Prevention and Other Health Benefits. Clin J Am Soc Nephrol. 2008;3:1548-54.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Vitamin D Insufficiency among Breast Cancer Survivors. Nutr Clin Pract. 2012;27:122-8.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D Insufficiency in a Multiethnic Cohort of Breast Cancer Survivors. Am J Clin Nutr. 2008;88:133-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of Vitamin D Supplementation along with Weight Loss Diet on Meta-inflammation and Fat Mass in Obese Subjects with Vitamin D Deficiency: A Double-blind Placebo-controlled Randomized Clinical Trial. Clin Endocrinol. 2019;90:94-101.
- [CrossRef] [PubMed] [Google Scholar]
- Review of Cancer from Perspective of Molecular. J Cancer Res Pract. 2017;4:127-9.
- [CrossRef] [Google Scholar]
- Mobile Genetic Elements: The Agents of Open Source Evolution. Nat Rev Microbiol. 2005;3:722-32.
- [CrossRef] [PubMed] [Google Scholar]
- Development and Reproduction in Humans and Animal Model Species Germany: Springer; 2015.
- [CrossRef] [Google Scholar]
- The Role of Nutritional and Environmental Alterations of Epigenetics on Human Health System. Eur J Volunteer Community Based Projects. 2022;1:38-51.
- [Google Scholar]
- Dysregulation of Histone Acetyltransferases and Deacetylases in Cardiovascular Diseases. Oxid Med Cell Longev. 2014;2014:641979.
- [CrossRef] [PubMed] [Google Scholar]
- The Role of Non-coding RNA (Ribonucleic acid) in the LC-Lung Cancer Pathogenesis System: ncRNA in Lung Cancer. Eur J Volunteer Community Based Projects. 2021;1:49-56.
- [Google Scholar]
- Effect of Non-Enzymatic Glycosylation in the Epigenetics of Cancer. Sem Cancer Biol. 2022;83:543-55.
- [CrossRef] [PubMed] [Google Scholar]
- The Developing Genome: An Introduction to Behavioral Epigenetics Oxford: Oxford University Press; 2015.
- [Google Scholar]
- Unravelling the Complexity of Metastasis-molecular Understanding and Targeted Therapies. Nat Rev Cancer. 2011;11:735-48.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Metabolic Syndrome, Vitamin D Level, and their Association among Elderly Women in a Rural Community of West Bengal, India. Med J Dr DY Patil Univ. 2020;13:315-20.
- [CrossRef] [Google Scholar]
- High Prevalence of Vitamin D Deficiency in Newly Diagnosed Acute Myeloid Leukemia Patients and Its Adverse Outcome. Int J Hematol Oncol Stem Cell Res. 2017;11:209-16.
- [Google Scholar]
- Hormone Receptor Expression in Multicentric/Multifocal Versus Unifocal Breast Cancer: Especially the VDR Determines the Outcome Related to Focality. Int J Mol Sci. 2019;20:5740.
- [CrossRef] [PubMed] [Google Scholar]
- Circulating Concentrations of Vitamin D in Relation to Pancreatic Cancer Risk in European Populations. Int J Cancer. 2018;142:1189-201.
- [CrossRef] [PubMed] [Google Scholar]
- Association of 25-OH Vitamin D Status with Findings on Screening Colonoscopy. Mil Med. 2018;183(Suppl 1):547-51.
- [CrossRef] [PubMed] [Google Scholar]
- Circulating Vitamin D Concentration and Risk of Prostate Cancer: A Dose-response Meta-analysis of Prospective Studies. Ther Clin Risk Manag. 2018;14:95-104.
- [CrossRef] [PubMed] [Google Scholar]
- Randomized Phase III Trial of Induction Chemotherapy with Docetaxel, Cisplatin, and Fluorouracil Followed by Surgery Versus Up-front Surgery in Locally Advanced Resectable Oral Squamous Cell Carcinoma. J Clin Oncol. 2013;31:744-51.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D Receptor Taq I Polymorphism and the Risk of Prostate Cancer: A Meta-analysis. Oncotarget. 2018;9:7136-47.
- [CrossRef] [PubMed] [Google Scholar]
- Associations between VDR gene Polymorphisms and Colorectal Cancer Susceptibility: An Updated Meta-analysis Based on 39 Case-control Studies. Oncotarget. 2018;9:13068-76.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D Receptor Polymorphism and Prostate Cancer Prognosis. Curr Urol. 2022;16:246-55.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D Receptor rs2228570 Polymorphism and Susceptibility to Ovarian Cancer: An Updated Meta-analysis. J Obstet Gynaecol Res. 2018;44:556-65.
- [CrossRef] [PubMed] [Google Scholar]
- Pharmacogenetics of the Anti-HCV Drug Sofosbuvir: A Preliminary Study. J Antimicrob Chemother. 2018;73:1659-64.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D Receptor Cdx-2 Polymorphism and Premenopausal Breast Cancer Risk in Southern Pakistani Patients. PLoS One. 2015;10:e0122657.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D and DBP: The Free Hormone Hypothesis Revisited. J Steroid Biochem Mol Biol. 2014;144:132-7.
- [CrossRef] [PubMed] [Google Scholar]
- Serum 25 (OH) D and Vitamin D Status in Relation to VDR, GC and CYP2R1 Variants in Chinese. Endocr J. 2014;61:133-41.
- [CrossRef] [PubMed] [Google Scholar]
- Genome-wide Association Study of Serum 25-hydroxyvitamin D in US Women. Front Genet. 2018;9:67.
- [CrossRef] [PubMed] [Google Scholar]
- Serum Vitamin D Metabolites in Colorectal Cancer Patients Receiving Cholecalciferol Supplementation: Correlation with Polymorphisms in the Vitamin D Genes. Horm Cancer. 2013;4:242-50.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D and Colon Cancer. World J Gastrointest Oncol. 2014;6:430-7.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D and Prostate Cancer Prognosis: A Mendelian Randomization Study. World J Urol. 2016;34:607-11.
- [CrossRef] [Google Scholar]
- A Polymorphism within the Vitamin D Transporter Gene Predicts Outcome in Metastatic Colorectal Cancer Patients Treated with FOLFIRI/Bevacizumab or FOLFIRI/Cetuximab. Clin Cancer Res. 2018;24:784-93.
- [CrossRef] [PubMed] [Google Scholar]
- Genetic Variation in Vitamin D-related Genes and Risk of Colorectal Cancer in African Americans. Cancer Causes Control. 2014;25:561-70.
- [CrossRef] [PubMed] [Google Scholar]
- CYP24A1 and CYP27B1 Polymorphisms Modulate Vitamin D Metabolism in Colon Cancer Cells. Cancer Res. 2013;73:2563-73.
- [CrossRef] [PubMed] [Google Scholar]
- The Associations between CYP24A1 Polymorphisms and Cancer Susceptibility: A Meta-analysis and Trial Sequential Analysis. Pathol Res Pract. 2018;214:53-63.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D Receptor-binding Site Variants Affect Prostate Cancer Progression. Oncotarget. 2017;8:74119-28.
- [CrossRef] [PubMed] [Google Scholar]
- Targeting Th17-IL-17 Pathway in Prevention of Micro-invasive Prostate Cancer in a Mouse Model. Prostate. 2017;77:888-99.
- [CrossRef] [PubMed] [Google Scholar]
- Interleukin-17A Promotes Lung Tumor Progression Through Neutrophil Attraction to Tumor Sites and Mediating Resistance to PD-1 Blockade. J Thorac Oncol. 2017;12:1268-79.
- [CrossRef] [PubMed] [Google Scholar]
- Toll-like Receptor 4 on Macrophage Promotes the Development of Steatohepatitis-related Hepatocellular Carcinoma in Mice. J Biol Chem. 2016;291:11504-17.
- [CrossRef] [PubMed] [Google Scholar]
- Investigating the Roles of Regulatory T Cells, Mast Cells and Interleukin-9 in the Control of Skin Inflammation by Vitamin D. Arch Dermatol Res. 2018;310:221-30.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D Supplementation for Improvement of Chronic Low-grade Inflammation in Patients with Type 2 Diabetes: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Nutr Rev. 2018;76:380-94.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of Long-term Vitamin D Supplementation on Regression and Metabolic Status of Cervical Intraepithelial Neoplasia: A Randomized, Double-blind, Placebo-controlled Trial. Horm Cancer. 2017;8:58-67.
- [CrossRef] [PubMed] [Google Scholar]
- Systems Analysis of the Prostate Transcriptome in African-American Men Compared with European-American Men. Pharmacogenomics. 2016;17:1129-43.
- [CrossRef] [PubMed] [Google Scholar]
- 1α 25-Dihydroxyvitamin D3 to Skew Intratumoral Levels of Immune Inhibitory CD34+ Progenitor Cells into Dendritic Cells. Otolaryngol Head Neck Surg. 2009;140:235-40.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D Supplementation Decreases Serum 27-hydroxycholesterol in a Pilot Breast Cancer Trial. Breast Cancer Res Treat. 2018;167:797-802.
- [CrossRef] [PubMed] [Google Scholar]
- Expression of Vitamin D Receptor and Vitamin D Status in Patients with Oral Neoplasms and Effect of Vitamin D Supplementation on Quality of Life in Advanced Cancer Treatment. Contemp Oncol. 2017;21:145-51.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D Supplementation and Survival in Metastatic Colorectal Cancer. Nutr Cancer. 2018;70:413-7.
- [CrossRef] [PubMed] [Google Scholar]
- Postmenopausal Breast Cancer Risk and Interactions between Body Mass Index, Menopausal Hormone Therapy Use, and Vitamin D Supplementation: Evidence from the E3N Cohort. Int J Cancer. 2016;139:2193-200.
- [CrossRef] [PubMed] [Google Scholar]






