Translate this page into:
Indirect Cost of Treatment of Tuberculosis: Could It be A Major Cause for Treatment Failure Leading to Emergence of Drug Resistant Tuberculosis?
Corresponding author: Umesh Chandra Ojha, Department Of Pulmonary Medicine, Employees State Insurance-Post Graduate Institute of Medical Sciences and Research, Delhi, E mail Id: ucojha@rediffmail.com
How to cite this article: Paul Choudhury E, Sarkar K, Ojha UC. Indirect Cost of Treatment of Tuberculosis: Could It be a Major Cause for Treatment Failure Leading to Emergence of Drug Resistant Tuberculosis? J Comprehensive Health 2020;8(2):33-37.
Abstract
Introduction:
Tuberculosis (TB) patients often incur huge costs due to TB care and the cost is even higher when it's an MDR-TB treatment. Despite free TB treatment under the Revised National Tuberculosis Control Program (RNTCP), the indirect cost borne by the patients due to the diagnosis and treatment of TB puts a major economic burden on the patients. This expenditure may affect treatment adherence and might lead to poor outcomes.
Method:
A cross-sectional study was conducted in a government health facility in Karimganj, Assam with 165 patients from the facility who were at least one month into the treatment. A pre-tested interviewer administered questionnaire on sociodemographic, clinical characteristics, and total cost due to TB care was recorded during the interview.
Result:
Out of 165 study participants, 52.7% belonged to the most productive age group of 19-54 years and 64.2% were male. The median indirect cost was INR 2333.33, which was higher than the direct cost and it contributes 96% of the total median cost. The indirect cost was significantly higher in patients who visited private facility first and patients having hypertension and diabetes. The indirect cost of treatment is significantly higher in MDR-TB patients when compared to non-MDR-TB patients.
Conclusion:
Even after the provision of free diagnosis and treatment under RNTCP, the indirect cost puts a major financial burden on the patients and their household, however, when it comes to MDR-TB patients, the burden is even bigger.
Keywords
Indirect cost
TB treatment
informal sector
domiciliarytreatment
Introduction:
Around the world, tuberculosis (TB) is among the top 10 leading causes of death. Globally, for about a quarter of TB burden is contributed by India with 2 million 800 thousand incidence cases. Worldwide, India is accounted for the second highest burden of MDR-TB after China with around new cases of 99,000 per year[1].
TB poses a major threat to socio-economic development in India. The estimated country's annual economic loss is US$ 3 billion, affecting the age group that is most economically productive (19-54) with more than 70% of cases[2]. Apart from that, an approximate of 170 million workdays are lost. According to the studies conducted, the direct and indirect cost of the disease is estimated to be 23.7 billion annually[3,4]. It is also interesting to note that India has 46.5 crore estimated work forces in the country and more than 90% of them are associated with informal economy sector or unorganised sector workers[5], who do not have even minimum social benefit and often come under economic exploitation. On the other hand, many of them are continuously exposed to respirable dust while working and vulnerable to dust related respiratory diseases such as silicosis. Vulnerable occupational groups include construction workers, rock mine workers, coal mine workers, agate workers, slate pencil workers etc. Workers exposed to silica are also vulnerable to tuberculosis, known as silico-tuberculosis due to continuous damage of lung macrophages by silica particles[6]. So, national TB control authority needs to focus on this issue for elimination of tuberculosis from the country.
Though the diagnosis and treatment of TB is free under Revised National Tuberculosis Control Programme (RNTCP), still a huge cost is incurred by TB patients on their illness and in the process to seek and receive healthcare, these costs appear to be even higher for some patients with additional morbidity. This cost, in turn, can create access and adherence barriers, thus affecting the health outcomes and shooting up the disease transmission risk and household's economic burden. It may also be noted that MDR-TB often has long term treatment seeking period of 24-27 months1 that might pose a greater financial involvement.
Considering above, a study was conducted to estimate the direct and indirect cost incurred by the various categories of patients due to tuberculosis. It was also intended to observe which factors determine the higher indirect cost for TB treatment with special reference to that of MDR-TB.
Methodology:
Study design
Hospital-based, cross-sectional, observational study conducted during December 2019 to April 2020.
Study participants
TB patients registered to a government health facility in Karimganj, Assam with minimum of 1 month into the treatment and who were willing to participate were included. Patient taking treatment from private practitioner, paediatric TB cases along with patients who were unwilling to participate were excluded from the study. Assam was chosen purposively. Assam has 33 districts out of which Karimganj was chosen conveniently. In Karimganj district, there are five Tehsils out of which Karimganj town was chosen conveniently.
Sample size
Considering the mean (SD) of the total cost incurred towards TB diagnosis and treatment as INR 3211 (535.47) from previous study[7], absolute precision of 100 units, 95% confidence interval, a sample size of 110 was obtained and as the cost data is generally skewed[8,9] so it was further increased by 50% by multiplying the obtained sample size with 1.5, the total sample size of 165 was obtained.
Data collection
The TB patients registered to a government health facility were interviewed with a pre-tested questionnaire administered to assess sociodemographic, clinical characteristics and the total cost. Cost data for last 30 days was recorded. Cost data was validated by questioning and cross checking with the existing rates wherever possible throughout the interview.
Definitions used
Direct medical costs are out-of-pocket costs incurred during medical care which includes registration, diagnostic tests, consultation to a physician, medication, paper work or to access any other health services[7]. Direct non-medical costs are those incurred during travelling to the health facility, their accommodation, food and any other expenditures[7]. Indirect costs are costs due to foregone earning because of inability to work due to the disease, lost time to visit a health facility, lost productivity, and job loss[10]. Coping costs measure the coping ways of a household to fulfil and meet the extra expenditure or income loss and by simultaneously meeting the daily household requirement. These include taking a loan, selling assets, savings lost, school dropouts to meet the expenses and taking another job to cope up the expenses[10].
Data analysis
Data was collated and cleaned in Microsoft Excel software then imported to STATA software. The analysis was conducted in STATA version 15.0. Study participants' characteristics were described and presented in the form of mean, median, percentage and frequencies, as applicable. The outcome variable was described and presented in the form of median (IQR).
Ethical consideration
This study was approved by the Institutional Ethics Committee of Indian Institute of Public Health, Delhi.

Out of 165, 81.21% belonged to the age group which is most productive (19-54), and 64.24% were male. Of all the participants, 43.03% of them were daily wage workers with 81.21% of them earning a per capita income of INR <5000. The median monthly earning of the patient was INR 9000 (0,18000) with a mean monthly household earning of INR 17000 (9500,23000).
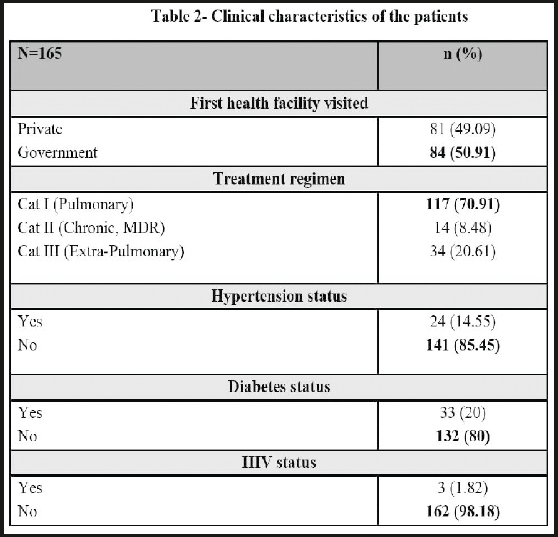
Among 165, 50.91% first visited government health facility with 70.91% of the patients getting treated under treatment regimen Cat I (Pulmonary TB). The treatment duration ranged from 1-17 months with a mean of 2.9 months. The mean time between first onset of symptom to first visit to a health facility (patient delay) was 22.31 (SD 18.80) days and the mean time between first consultation to diagnosis (provider delay) was 9.8 (SD 5.61) days. Coping cost includes loan of median (IQR) INR 5000 (4000,6000) taken by 6.67% of the participants and loss of the median (IQR) saving of INR 2000 (700,3000). No mortgage or sale was done by any of the participants in the study.
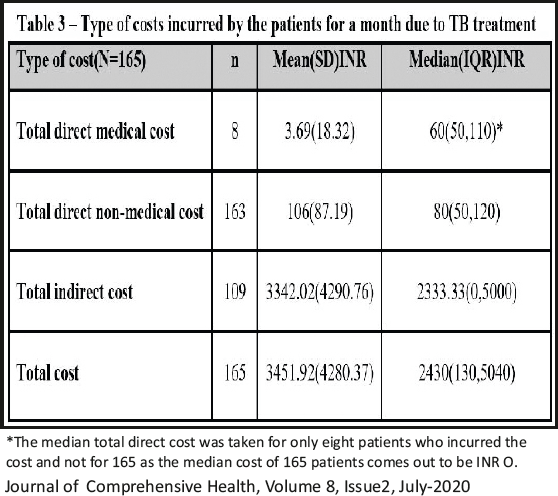
The direct medical cost was incurred by only 4.84% patients costing them a median of INR 60. The direct non-medical cost was incurred by 98.78% patients costing them a median of INR 80. The indirect cost was the major cost borne by the patients with 66.06% patients bearing it. The indirect cost captured in this study was the income loss due to TB care. Four patients had lost their jobs after the episode of TB and two out of four were MDR-TB patients.
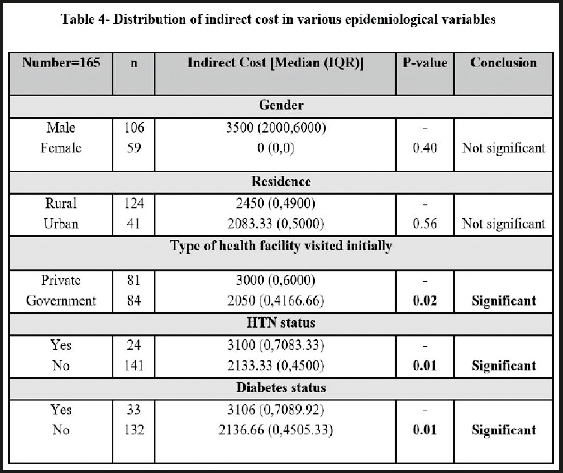
After applying a simple linear regression, it was confirmed that the total cost was significantly higher in patients who visited private facility initially (p-value 0.02) and patients with co-morbidities like hypertension (p-value 0.01) and diabetes (p-value 0.01). However, the same were not significant anymore when multivariable linear regression was applied.
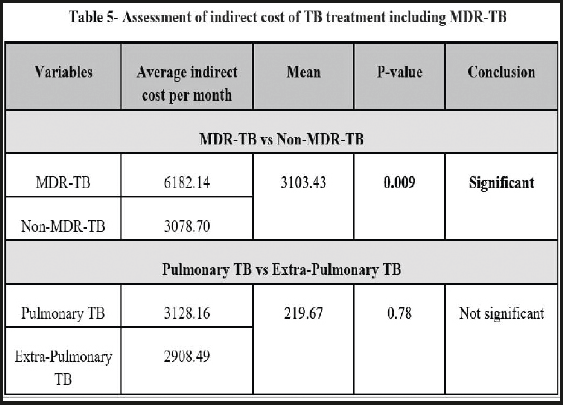
It was found that there is significant difference between indirect costs of MDR-TB and non-MDR-TB patients. Although, the difference came out to be insignificant for pulmonary and extra-pulmonary TB patients as shown in table-5.
Discussion:
This study shows that a higher indirect cost was borne by the males as compared to females, though this factor came out to be not significant as shown in table-4. Similar observation was observed by another study that found the male to be a predictor of higher cost of treatment[11]. Observations of two other Indian studies are also consistent with this study findings[7,9]. This is because of the fact that males are generally the sole bread-earners in many families, as a result, loss of income increases due to absenteeism and wage loss. Contrarily, a study from Zambia had found that when a woman seeks TB care, the opportunity cost incurred by the household was greater and they also pay higher direct cost as proportion of their earning[12]. When compared to the patients in urban areas, patients from rural areas spend a higher indirect cost but that difference was not statistically significant. Although, a study from Nigeria reported about rural residence to be a determinant of household poverty for seeking TB treatmentll. This happens because the patients from rural areas need to travel from far off places and paid leave is hardly an option for them which surges up their indirect cost along with out-of-pocket expenses.
The present study documents that a sizable portion of patients visited private health facilities first, paying higher treatment cost. In contrast, some visited government facilities directly. The cost difference of both facilities is statistically significant as evidenced in table-4. In private facilities, unnecessary and excessive investigations, medications and symptomatic treatment increases the cost often. Inappropriate drug regimens were prescribed by many with incorrect combinations and faulty doses for wrong duration as observed[13]. Expenses in private facility are often higher when compared to the government facility[14]. A systemic review in sub-Saharan Africa of patients' cost have recorded the same among others and opined that seeking care from private sector is an important driver which lead to catastrophic costs[15].
Patients with co-morbidities like hypertension and diabetes are associated with higher indirect cost because an additional co-morbidity makes the patient sicker often. In this study, differences were found significant both in hypertension as well as diabetes (table-4). A study from Malaysia had also evidenced an increasing treatment cost and hospitalization period when diabetes was present as a co-morbidity along with TB[16].
The median total cost for monthly TB care was INR 2430/- in this study (Table-3). The direct medical cost was incurred by only 8 patients requiring hospitalization fees as RNTCP advices domiciliary treatment which avoids hospitalization of the patients and reduces the medical cost. The direct nonmedical cost was incurred by 163 patients which was incurred due to spending for travelling to the health facility and fooding. The direct medical and direct non-medical cost accounted for 2.46%, 3.29% of the total median cost, respectively. The overall median direct cost estimated for a month is INR 140/-. In India, a study among tribal population, estimated a median direct cost of INR 1105/- and 86% patients didn't bear any direct cost[17]. It may be noted that the overall median direct cost in the study was less than the previous studies[7,8,17,18]. Therefore, it suggests that overall DOTS save the medical expenses of the households.
This study shows an average monthly indirect cost INR 6182 for MDR-TB as compared to the same of non-MDR-TB of INR 3078 per month. This difference is statistically significant as shown in table-5. This indicates that each MDR-TB patient needs to spend on an average Rs. 6182 (almost double the monthly amount of non-MDR-TB). Considering their monthly income and daily wage loss for seeking TB treatment, it appears to be a huge burden for both the non-MDR-TB as well as MDR-TB. Indirect cost of MDR-TB accounts for 68.69% of monthly individual earning and 36.36% of monthly household earning which is exorbitantly higher as observed in this study and it could be a major concern for continuation of their treatment till the required duration. Failure of continuation of MDR-TB due to cost constraints will lead to increase of MDR-TB, which must be adequately taken care of by the national TB control authority. Similarly, no significant cost difference was observed between pulmonary and nonpulmonary TB in this study. A study from Chennai had reported a median total indirect cost INR 745 which contributed for the major portion of the total cost which was INR 16157. A study from Zambia reported 48 days' average income loss due to TB care19. Another study from Nigeria has reported a higher indirect cost of US$ 416 which accounts for 79% of the total median cost and 52% of median annual patient earning[11]. A concerning finding was that the indirect cost of MDR-TB patients was significantly higher compared to non-MDR-TB patients as discussed above. This was because of the frequent visits to the health facility and hospitalization. The MDR-TB treatment also lasts for longer period compared to non-MDR-TB. Another study had also observed high indirect cost because of longer treatment duration of MDR- TB20. Even after decentralization of DOT, patients need to incur high indirect cost due to wage loss, as many of them need to travel a long distance to seek TB care. This clearly indicates that this strategy may not work efficiently and needs suitable re-structuring to avoid treatment failure and consequent emergence of more and more drug resistant tuberculosis in the community. Limitations of this study are biases associated with self-reported behaviours such as inflated estimation of treatment seeking cost, underevaluating income information, lack of generalizability of the study as it was conducted in population residing in and around a small town, limitation of income data analysis as some of the participants' indirect cost could not be calculated as they have no formal income (such as students, housewives etc) in spite of their expenditure like others.
References:
- Challenges and Potential Solutions: Summary of a Joint Workshop by the Institute of Medicine, the Indian National Science Academy, and the Indian Council of Medical Research. National Academies Press (US) 2012 https://www.ncbi.nlm.nih.gov/books/NBK100386/ (accessed )
- [Google Scholar]
- India's Revised National Tuberculosis Control Programme (RNTCP): Budget and Performance. Journal of Health Management (3):261-271. https://dhr.gov.in/ sites/default/files/India%E2%80%99s%20Revised%20N ational%20Tuberculosis%20Control%20P.pdf (accessed )
- [CrossRef] [Google Scholar]
- Central Tuberculosis Division. https://tbcindia.gov.in/index1.php?lang=1&level=1&su blinkid=4160&lid=2807 (accessed )
- [Google Scholar]
- Indirect cost as hindrance in availing DOTS for Tuberculosis: Is the treatment truly free of cost? National Journal of Medical Research. 2012;2(1):35-38. https://www.bibliomed.org/?mno=18647 (accessed )
- [Google Scholar]
- Unorganised Workers: A Core Strength of Indian Labour Force: An Analysis. International Journal of Research in Business Studies and Management. 2015;2(12):44-56. https://www.ijrbsm.org/pdf/v2-i12/6.pdf (accessed )
- [Google Scholar]
- Club cell protein 16 as a biomarker for early detection of silicosis. Indian Journal of Medical Research. 2020;151(4):319. https://pubmed.ncbi.nlm.nih.gov/32461395/ (accessed )
- [CrossRef] [PubMed] [Google Scholar]
- Expenditure Pattern for TB Treatment among Patients Registered in an Urban Government DOTS Program in Chennai City, South India. Tuberculosis Research and Treatment 2012 Article ID 747924. https://www.hindawi.com/journals/trt/2012/747924/ (accessed )
- [CrossRef] [PubMed] [Google Scholar]
- Catastrophic costs of tuberculosis care: a mixed methods study from Puducherry, India. Global Health Action. 2018;11(1):1477493. https:// pubmed.ncbi.nlm.nih.gov/29902134/ (accessed )
- [CrossRef] [PubMed] [Google Scholar]
- Identifying costs contributing to catastrophic expenditure among TB patients registered under RNTCP in Delhi metro city in India. Indian Journal of Tuberculosis. 2019;66(1):150-157. https://doi.org/10.1016/j.ijtb.2018.10.009 (accessed )
- [CrossRef] [PubMed] [Google Scholar]
- Tool to estimate Patient's cost. http://www.stoptb.org/wg/ dots_expansion/tbandpoverty/assets/documents/Tool %20to%20estimate%20Patients'%20Costs.pdf (accessed )
- [Google Scholar]
- The High Cost of Free Tuberculosis Services: Patient and Household Costs Associated with Tuberculosis Care in Ebonyi State, Nigeria. PLoS ONE. 2013;8(8):e73134. https://doi.org/10.1371/journal.pone.0073134 (accessed )
- [CrossRef] [PubMed] [Google Scholar]
- Cost of tuberculosis diagnosis and treatment from the patient perspective in Lusaka, Zambia. Int J Tuberc Lung Dis. 2008;12(8):928-35. Available through: https://pubmed.ncbi.nlm.nih.gov/18647453/ (accessed )
- [Google Scholar]
- Private practitioners and public health: weak links in tuberculosis control. Lancet. 2001;358(9285):912-6. https://www.ncbi.nlm.nih.gov/pubmed/11567729 (accessed )
- [CrossRef] [PubMed] [Google Scholar]
- From Where Are Tuberculosis Patients Accessing Treatment in India? Results from a Cross-Sectional Community Based Survey of 30 Districts. PLoS ONE. 2011;6(9):e24160. https://doi.org/10.1371/journal.pone.0024160
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculosis and poverty: the contribution of patient costs in sub-Saharan Africa - a systematic review. BMC Public Health. 2012;12(1):980. http://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-12-980last (accessed )
- [CrossRef] [PubMed] [Google Scholar]
- Economic Burden of Diabetic Tuberculosis Patients. British Journal of Medicine & Medical Research. 20132013;3(4):1598-1606. https://www.researchgate.net/publication/264775482_ Economic_Burden_of_Diabetic_Tuberculosis_Patientsla st (accessed )
- [CrossRef] [Google Scholar]
- Household Catastrophic Health Expenditure Due To Tuberculosis: Analysis From Particularly Vulnerable Tribal Group, Central India. Med Mycol Open Access. 2015;2:9. https://mycology.imedpub.com/household-catastrophic-health-expenditure-due-to- tuberculosis-analysis-from-particularly-vulnerable-tribal-group-central-india.php?aid=7846 (accessed )
- [CrossRef] [Google Scholar]
- Cost incured by the patient with pulmonary Tuberculosis in rural India. Int J Tuberc Lung Dis. 2009;13(10):1281-1287. https://sci-hub.tw/https://www.ingentaconnect.com/content/iuatld/ijtld/2009/00000013/00000010/art00016 (accessed )
- [Google Scholar]
- Barriers to tuberculosis control in urban Zambia: the economic impact and burden on patients prior to diagnosis. International Union Against Tuberculosis and Lung Disease. 1998;2(10)International Union Against Tuberculosis and Lung Disease. 1998;2(7):811-817. https://www.ingentaconnect.com/content/iuatld/ijtld/1998/00000002/00000010/art00008 (accessed )
- [Google Scholar]
- Costs of patients hospitalized for multidrug- resistant tuberculosis. Int J Tuberc Lung Dis. 2004;8(8):1012-6. https://pubmed.ncbi.nlm.nih.gov/15305486/ (accessed )
- [Google Scholar]






