Translate this page into:
Human Immunodeficiency Virus Status Disclosure and Associated Factors among Children in the Pediatric Anti-Retroviral Therapy Clinic at Gambella Public Hospitals, Gambella Region, Southwest Ethiopia
*Corresponding author: Abebe Ejigu Desta, Department of Epidemiology, Faculty of Public Health, Jimma University, Jimma, Ethiopia. abebeejigu7@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Desta AE, Mengesha CH, Mogas SB. Human Immunodeficiency Virus Status Disclosure and Associated Factors among Children in the Pediatric Anti-Retroviral Therapy Clinic at Gambella Public Hospitals, Gambella Region, Southwest Ethiopia. J Compr Health. 2025;13:54-64. doi: 10.25259/JCH_46_2024
Abstract
Background
Globally, 1.7 million children are estimated to be living with HIV. As highly active antiretroviral therapy becomes progressively available in low resource settings, children are living longer and having longer survival times. Thus, one of the greatest psychosocial challenges that caregivers face is HIV- positive status disclosure to children which is becoming a common issue in clinical practice.
Objectives
To assess the magnitude and associated factors of disclosure among HIV- positive children in public hospitals in the ART clinic in Gambella town.
Material and Methods
A facility- based cross- sectional study was performed using quantitative and qualitative data collection methods. The study was performed from March 10 to April 15, 2020 among 259 HIV- infected children aged 6-18 years and their caregivers in two public hospitals, in Gambella town. Bivariate and multivariate logistic regression analyses were applied to determine the factors associated with HIV status disclosure with a P-value <0.05 and a 95% confidence interval of the Adjusted odds ratio (AOR).
Results
Ninety-eight (37.8%) HIV-positive children were informed of their status. Biological fathers (AOR=5.37; 95%CI=2.18, 13.21); biological mothers (AOR=3.65; 95%CI=1.64, 8.15), and children aged ≥10 years (AOR=3.73; 95%CI=1.47, 9.49), duration of ART (11-16 years) (AOR=4.15; 95 %CI=1.55, 11.13) and adherence to ART treatment of child; good(AOR=3.33; 95%CI= 1.81, 6.13) were found to be significantly associated with HIV positive status disclosure to children.
Conclusion
The magnitude of disclosure of HIV- positive status to infected children was low. Caregiver’s relation with child, age of the child, duration of ART and adherence to ART treatment were associated with the disclosure of HIV-positive status in infected children. Therefore, age appropriate counseling and working on related factors are important for improving low disclosure.
Keywords
Caregiver
Children
Disclosure
Gambella town
Human immunodeficiency virus
INTRODUCTION WITH OBJECTIVES
The human immunodeficiency virus (HIV) has become one of the world’s most serious health and development challenges, worldwide as it has a disturbing impact on adults and children.1 Globally, of the estimated 37.9 million people living with HIV (PLWH)/acquired immunodeficiency syndrome (AIDS) in 2019, 1.7 million were children.2 Of these, 25.9 million people were living in Africa, 70% were living in Sub-Saharan Africa (SSA), 54% were living in eastern and southern Africa, and more than 88% were children but only 13% of the world’s population found in Africa.1,2 More than 50% of PLWH in SSA are women and children; this is why they are still indistinct and destructive.3 Most children are infected by their HIV-infected mothers during pregnancy, childbirth, or breastfeeding.4,5 In Ethiopia, there were 690,000 PLWH; of these, 36,000 lived with HIV and in the Gambella region, 12,347 PLWH were estimated to have lived in 2017.6
Disclosure was defined as a state in which a child gained knowledge about his/her HIV-positive status.7 It is key not only enter to treatment but also to prevent transmission and receive support from healthcare providers, family, and friends for one’s disease.8 As highly active anti-retroviral therapy (ART) is progressively available in low-resource settings, children are living longer and having improved survival. One of the psychosocial challenges that caregivers face is disclosing HIV-positive status to children, and another challenge is when and how to inform them and this is becoming a common issue in clinical practice.8,9 However, in 2011, the World Health Organization (WHO) developed guidelines, and the Ethiopian Ministry of Health comprehensive HIV treatment guidelines recommended that HIV-positive children should be disclosed at school age. This should be planned incrementally to age-appropriate information and cognitive skills of the child. However, caregivers worry about accepting the illness, either their own or their child’s, and struggle with whether or not to disclose it and fear the consequences.10,11 Therefore, healthcare providers and other member teams should collaborate with caregivers of children to disclose HIV diagnosis to the child in a developmentally proper way.12
The HIV pandemic is the most severe public health challenge facing the world to date and has serious economic implications, especially in highly prevalent regions such as SSA including Ethiopia.13 This burden not only affects the health of individuals but also has impacts on the family, community, and economic growth of nations.1 In the past 15 years, there has been a 35% decrease in global HIV infections at all ages and a 58% decrease in HIV infections in children, but more than 54% of children are currently infected because they are unaware of the disease. Therefore, disclosure rates in regions with high HIV should be evaluated and improved drastically in a timely manner. Disclosure may be a key factor in reducing the risk of acquiring new infections, improving adherence, and practicing safe sexual behaviors.14 Despite the decrease in HIV transmission from mother to child, new cases are diagnosed every day as a result, caregivers fear the guilt and shame of disclosing the virus.15
The provision of comprehensive treatment for HIV/AIDS with increased availability and use of cost-effective anti-retroviral (ARV) drugs has a significant positive impact on HIV-infected children. As a result, children who live longer with HIV as a chronic illness progress to adolescence and adulthood. Therefore, HIV-positive disclosure is important when considering age-appropriate cognitive development.16 The WHO recommended that children disclose at school age and above (6 years and above) and plan incrementally to age-appropriate information, their cognitive skills, and emotional maturity. However, caregivers have trouble accepting the illness, either their own or their child’s, and struggle with whether or not to disclose it and fear the consequences.11 However, disclosure is still challenging even if it has proven to have numerous social and medical benefits for the child and families.17
A longer duration of treatment for children on ART brings new challenges; the issue of disclosure becomes more important because of the multiple benefits: Improving psychosocial and clinical outcomes; adhering to ART, remaining in care, and promoting safer sexual practices to prevent secondary transmission.18,19 However, caregivers are reluctant to disclose; because they fear stigma and discrimination, a parental sense of guilt and shame, a child who is too young to cope with stress and/or fear that children will not keep the diagnosis, children who are losing their friends and social standing in schools.4,15,20
Covering HIV status disclosure on the other hand may exacerbate depression, worry, and other negative mental health outcomes, potentially interfering with treatment and affecting family life such as parenting ability and children’s social and academic life.11 If this is allowed to continue, it would have negative consequences not only for children but also for the entire country because it would lead to poor treatment adherence. As a result, poor treatment outcomes include treatment failure; increased drug resistance; potential transmission of drug-resistant viruses to sexual partners through unprotected sex while they become adolescents; increased risk of HIV transmission to the general population; increased risk of early disease progression, and decreased survival time.21 Therefore, to improve disclosure, there is a need to understand the locally prevalent perceptions of caregivers and the influencing factors of HIV status disclosure to children are important in the treatment of infected children.15,22
Although the WHO recommends HIV-positive status disclosure for infected children, studies have shown that the prevalence of HIV-positive status disclosure varies from 10% to 77% in resource-rich countries and 13% to 60% in low and middle-income countries.14,19 A systematic literature review of SSA revealed that the prevalence of these diseases ranged from 9% to 72%.4 This shows that disclosure is quite low, particularly in SSA countries including Ethiopia, and that disclosure has received relatively little attention, but 88% of children living with HIV (CLWH) are found in Africa.4,23
A study performed in SSA showed that closed children were more likely to become depressed, feel worried, have a decreased cluster of differentiation 4 (CD4) count, and have a decreased survival time.4,24 Despite the recognized benefits of disclosure, many infected children in most resource-limited settings including Ethiopia do not know their status and this vital information should be provided by caregivers promptly.25
Adolescents have to make decisions about idealistic relationships, and sexual activities, test alcohol consumption, and plan for the future. However, these choices can be made only with an appropriate understanding of their HIV status and the nature of it. Since they are more likely to have sex before the age of 15 or 18 years, they are at risk of pregnancy and sexually transmitted infections including HIV/AIDS.26 Studies performed in Ethiopia showed that the prevalence of disclosure ranges from 17.4% to 49.4%.9,12,24,27,28 As a result, low disclosure causes a severe effect on children who are not aware of their HIV-positive status and may remain less likely to take their medication regularly, which can lead to drug resistance, exposure to different opportunistic infections, and decreased survival time. Hence, it is important to determine the prevalence of disclosure, its associated factors, and the experience of caregivers to design appropriate interventions suitable for specific study areas. Therefore, this study aimed to address this gap by determining the prevalence of HIV status disclosure and associated factors among children aged 6–18 years in pediatric ART clinics at Gambella town public hospitals, in Southwest, Ethiopia.
MATERIAL AND METHODS
Study area and period
The study was conducted in Gambella people’s National Regional state, Gambella town public hospitals that provide pediatric ART services. This region is one of the ten regions in Ethiopia and Gambella town is the capital city of the region and is located 771 Km southwest of Addis Ababa, the capital city of Ethiopia. The town is founded on the bank of the Barro River, Ethiopia’s widest and only navigable river. According to the town health bureau report, the estimated population in 2019 was 61,378. The town has two public hospitals: General and primary hospitals. There were 2355 HIV clients in Gambella General Hospital; of these, 546 were children and 247 were HIV clients in Gambella Primary Hospital; of these, 113 were children aged 6–18 years. The study was conducted from March 10 to April 15, 2020 (Ministry of Health (MOH) Ethiopia District Health Information Software vesion 2 [DHIS2]).
Study design
A facility-based cross-sectional study was designed using both quantitative and qualitative data collection methods.
Population
All HIV-positive children aged 6–18 years in the town of the Gambella region were the study population. Moreover, HIV-positive children aged 6–18 years with their caregivers regularly visiting two public hospitals in pediatric ART clinics fulfilled the inclusion criteria. The respondent population was caregivers whose age >18 years with their HIV-positive children. Moreover, caregivers’ children aged 6–18 years were diagnosed with HIV before 6 months and follow-up visits in pediatric ART clinics in the two public hospitals were included in this study. Caregivers of children who could not communicate were or seriously ill were excluded.
Sample size determination
The sample size was calculated using the single population proportion formula by considering the following assumptions: 5% margin of error, 95% confidence level, and 44% estimated prevalence of HIV-positive status disclosure among CLWH.24 Since the source population was 659, the finite population correction formula was applied. After adding a non-response rate of 10%, the final sample size was 265.
Sampling procedures
The study was conducted in the pediatric ART clinics of two public hospitals (general and primary hospitals) providing ART services to Gambella town using a stratified sampling technique. The data of HIV-infected children aged 6–18 years who were currently on follow-up were obtained from the ART registration document of each of the general and primary hospitals. The sample size was proportional to the population size by the total number of HIV-infected children sampled at the two selected hospitals. Finally, the respondents were selected by a systematic sampling technique. For a caregiver who had more than one child, information was reported for only one randomly selected child [Figure 1].
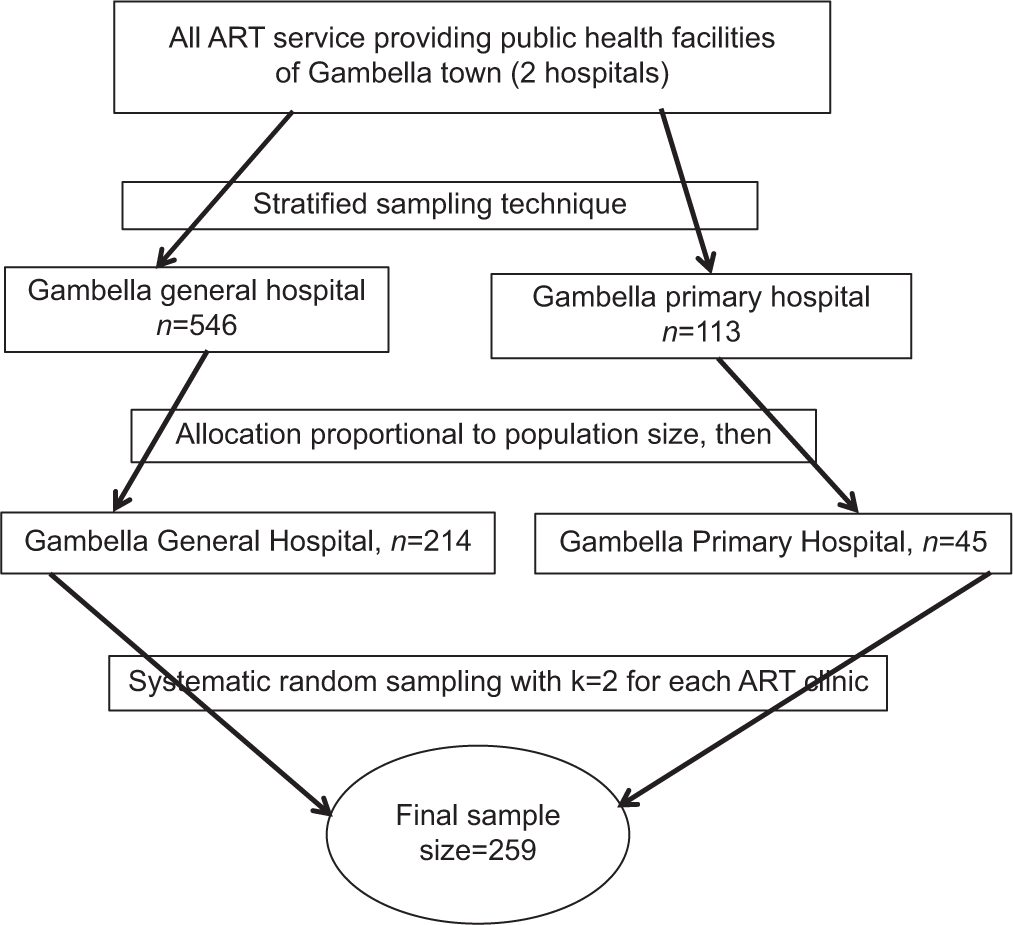
- Schematic presentation of sampling procedures for selecting participants at public hospitals in Gambella town, Southwest Ethiopia, 2020 (n = 259). ART: Anti-retroviral therapy.
For qualitative data, caregivers of HIV-infected children and healthcare providers were selected purposively based on previous experience with HIV disclosure. Eight caregivers (four caregivers from each hospital) were selected from different localities since they might have different disclosure experiences and four healthcare providers (two from each hospital) in two hospitals in the town were included.
Operational definitions
Disclosure
When the caregiver said that the child now knows their HIV/AIDS diagnosis, it did not matter who had revealed the information.24,28
Caregivers were those aged older than 18 years, who participated in the child’s daily care and who knew most about the child’s health.24,29
ART adherence
It was measured based on the number of missed doses within 30 days. Thus, three or fewer missed doses (≥95%) were rated as good, four to eight missed doses (85–94%) were rated as fair, and nine or more missed doses (<85%) were rated as poor.30
Caregivers’ knowledge
If the caregiver correctly responded more than the median score from nine items HIV-related questions, then he/she had good knowledge; otherwise; he/she had poor knowledge.
Data collection procedures
A semi-structured face-to-face interview questionnaire was adapted after reviewing the related literature for a quantitative study.5,24,28,31 The questionnaire was first written in English, subsequently translated into the local language Amharic by experts, and subsequently back-translated into English by other experts to check its consistency. The survey contained information on sociodemographic characteristics and clinical, sociocultural, and individual factors of the caregiver and child. Caregivers’ HIV knowledge was assessed using nine (9) item questions. To calculate the median score for caregiver’s HIV knowledge, each item was computed as “yes” (1) was considered correct and those computed as “no and I do not know” and (0) were considered incorrect. Therefore, caregiver knowledge was calculated using these items and the median score was used to classify knowledge as good or poor. For qualitative data, a semi-structured interview guide was used for key informant interviews, and in-depth interviews were used to support the quantitative study. In addition, tape audio records were used. The data were collected by two trained Bachelor of Science nurses and public health officers for supervisors from the two public hospitals. For qualitative data, caregivers and healthcare providers were interviewed by the principal investigator. Quantitative data were collected through face-to-face interviews using a semi-structured questionnaire. Five percent of the study participants were pre-tested at the Dimma Health Center. The interview took place after participants had attended their ART follow-up visit.
The responsibility of the data collector was to explain to each caregiver the purpose of the study and the confidentiality of the information. To prevent accidental HIV status disclosure to the children, clients were separated from their caregivers during the data collection after which the clients were subjected to face-to-face interviews after consent was obtained from the caregivers. Secondary data were reviewed from records using checklists for the WHO clinical stage, recent CD4 count, viral load, and treatment adherence. For in-depth interviews and key informant interviews, a semi-structured interview guide was used to interview participants to explore and understand their perceptions and experiences of attitudes toward disclosure of HIV-positive status to infected children. Interviews were facilitated by a principal investigator using a guide and tape audio records were obtained with the participant’s permission. Notes were taken by the principal investigator and four key informant interviews and eight IDIs were held until information saturation was reached.
Data quality control
The questionnaires were translated from English into the Amharic language by experts and backtranslated into English by other experts to check the consistency. The data collectors and supervisors were trained on the objectives, contents, and procedures of the data collection before the actual study was started by the principal investigator. The questionnaire was pre-tested at Dimma Health Center by taking 5% of study the participants before the actual study to assess clarity, flow, completeness, skip patterns, and internal consistency, then revisions were performed before data collection. The internal consistency reliability of the caregiver’s HIV knowledge questionnaire was checked using Cronbach’s alpha which was 0.7. The key informant interviews and in-depth interviews were tape-recorded and transcribed on the same day after data collection and appropriate corrections were made for the next day. The principal investigator and supervisors conducted daily data monitoring for completeness, corrected mistakes, and checked errors.
Data processing and analysis procedure
The data were edited and coded manually by a principal investigator. The data were subsequently, entered into Epidata software version 3.1, and exported to the Statistical Package for the Social Sciences version 25 software for data cleaning, categorization, and recoding before analysis. Then, descriptive analysis was performed to describe the sociodemographic characteristics of the caregivers and children; thus, the frequency and percentage were computed for categorical variables and the mean or median was computed for continuous variables. HIV-positive status disclosure to the child was dichotomized as disclosed (yes = 1) or not disclosed (no = 0) based on caregivers’ self-reports.
Bivariate analysis was performed to identify candidate variables for multivariate analysis using a P < 0.25. Multivariate binary logistic regression analysis was carried out to control for possible confounding variables and identify factors independently associated with the disclosure of HIV-positive status in children. The backward stepwise variable selection method was used in multivariate analysis. Model adequacy was checked using the Hosmer and Lemeshow goodness-of-fit test (P = 0.97). A P < 0.05 and 95% CI for the AOR were considered to indicate a statistically significant association in the final model. Finally, the results are presented in texts, tables, and graphs.
For the qualitative data, the recorded data were transcribed precisely and then translated into English word by word. Thematic analysis was performed by sorting information, identifying similarities and differences, and developing appropriate codes. Finally, the data were summarized and direct quotations were used to present the data along with the quantitative findings.
RESULTS
Sociodemographic and clinical characteristics of caregivers of HIV-positive children
A total of 259 caregivers of HIV-positive children participated in the study with a response rate of 97.7%. Two-thirds, 173 (66.8%) were female caregivers, 193 (74.5%) were biological caregivers of children, and the mean age of the caregivers was 39 years (Standard deviation [SD] = 7.3 years). HIV status of 170 caregivers of the 237 tested was negative (>50%) and the source of infection might be exposed after delivery from another source but caregivers feel guilty during disclosure, since they considered their children ask them the source of infection and might not keep secret [Table 1].
| Variables (n=259) | Frequency | Percentage |
|---|---|---|
| Age of caregivers | ||
| 19–30 | 39 | 15.1 |
| 31–40 | 122 | 47.1 |
| 41–50 | 87 | 33.6 |
| ≥51 | 11 | 4.2 |
| Sex | ||
| Male | 86 | 33.2 |
| Female | 173 | 66.8 |
| Marital status | ||
| Married | 177 | 68.3 |
| Single | 21 | 8.1 |
| Widowed | 40 | 15.4 |
| Divorced | 21 | 8.1 |
| Level of education | ||
| Not able to read and write | 36 | 13.9 |
| Primary (grade 1–8) | 80 | 30.9 |
| Secondary (grade 9–12) | 63 | 24.3 |
| Tertiary (above grade 12) | 80 | 30.9 |
| Family size | ||
| <3 | 15 | 5.8 |
| ≥3 | 244 | 94.2 |
| Occupational status | ||
| Farmer | 20 | 7.7 |
| Government employer | 96 | 37.1 |
| Merchant | 98 | 37.8 |
| Daily laborer | 22 | 8.5 |
| Other | 23 | 8.9 |
| Caregivers’ relation with child | ||
| Father | 59 | 22.8 |
| Mother | 134 | 51.7 |
| Grandparent | 16 | 6.2 |
| Relative | 50 | 19.3 |
| HIV test status of caregivers | ||
| No | 22 | 8.5 |
| Yes | 237 | 91.5 |
| HIV test result | ||
| Positive | 66 | 25.5 |
| Negative | 170 | 65.6 |
| Unknown | 23 | 8.9 |
HIV: Human immunodeficiency virus, ART: Anti-retroviral therapy
Sociodemographic and clinical characteristics of HIV-positive children
A total of 259 HIV-positive children aged 6–18 years whose caregivers participated in the study were included and the mean age of the children was 11.5 years (SD = 3.4 years) [Table 2].
| Variables (n=259) | Frequency | Percentage |
|---|---|---|
| Mean age±SD (in years) | 11.52±3.4 | |
| Age | ||
| <10 | 81 | 31.3 |
| ≥10 | 178 | 68.7 |
| Sex | ||
| Male | 151 | 58.3 |
| Female | 108 | 41.7 |
| Educational level | ||
| Not started | 33 | 12.7 |
| KG | 21 | 8.1 |
| Primary (grade1–8) | 174 | 67.2 |
| Secondary (grade 9–12) | 31 | 12.0 |
| Age at HIV diagnosis | ||
| <5 | 209 | 80.7 |
| ≥5 | 50 | 19.3 |
| Age of the child when ART initiated | ||
| 1–5 | 201 | 77.6 |
| 6–11 | 56 | 21.6 |
| ≥12 | 2 | 0.8 |
| Duration on ART | ||
| 1–5 | 94 | 36.3 |
| 6–10 | 107 | 41.3 |
| 11–16 | 58 | 22.4 |
| Child’s responsible to his/her drugs? | ||
| No | 93 | 35.9 |
| Yes | 166 | 64.1 |
| Loss of biological caregivers due to HIV? | ||
| No | 198 | 76.4 |
| Yes | 61 | 23.6 |
| Recent CD4 count | ||
| <500 | 52 | 20.1 |
| ≥500 | 207 | 79.9 |
| Recent viral load | ||
| ≤1000 | 210 | 81.1 |
| >1000 | 49 | 18.9 |
| Recent WHO HIV clinical stage | ||
| Stage 1 | 130 | 50.2 |
| Stage 2 | 81 | 31.3 |
| Stage 3 | 34 | 13.1 |
| Stage 4 | 14 | 5.4 |
| Recent ART treatment adherence | ||
| Good | 137 | 52.9 |
| Fair | 101 | 39.0 |
| Poor | 21 | 8.1 |
SD: Standard deviation, KG: Kindergarten, HIV: Human immunodeficiency virus, ART: Anti-retroviral therapy, CD4: Cluster of differentiation 4, WHO: World Health Organization
HIV-positive status disclosure to infected children
According to the caregiver’s response to their children’s HIV-positive status disclosure, only 98 (37.8%; 95% confidence interval [CI]: 31.9%, 44.0%) of the children disclosed their HIV-positive status. Of these, 84 (85.7%) of the children knew the name of the virus. The median age of the children at disclosure was 10 years (interquartile range = 1 year), and 87 (88.8%) were 10 years or older. More than half of the participants (54) (55.1%) were male, 92 (93.9%) had attended primary education and above, and 66 (67.3%) were disclosed by their biological caregivers; of these, 50 (51%) were biological mothers. One hundred eight seven (72.2%) of caregivers of HIV-positive children had good knowledge of HIV.
Reasons why caregivers disclose HIV-positive status to infected children
Caregivers stated the main reasons for disclosing their HIV-positive children in this study. Most, 71 (72.4%) of the caregivers stated that children asked repeated questions about their health conditions, and 67 (68.4%) of them mentioned that the child was mature enough to understand the illness [Figure 2].
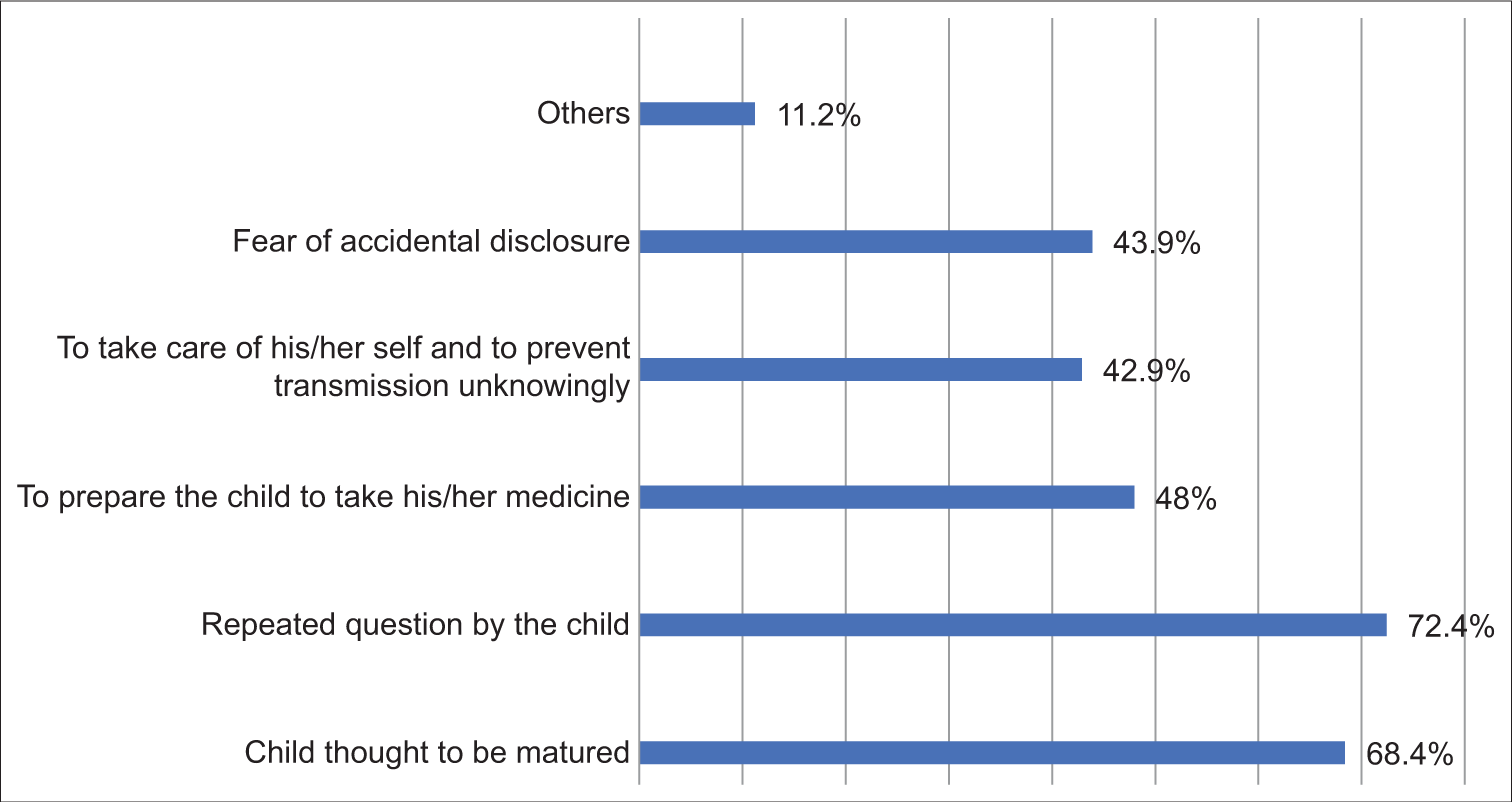
- Caregivers’ reasons for disclosing human immunodeficiency virus-positive status to infected children in pediatric anti-retroviral therapy clinic at Gambella town public hospitals, Ethiopia, 2020 (n = 259 ). Others: Includes right to know his/her disease condition and to share responsibility. Total percentage exceeds 100% because multiple responses were possible. X-axis-Caregivers responses measuerd by proportion (%), Y-axis -Caregivers reasons for disclosing HIV.
Based on our qualitative study findings; “I disclosed my child because health care providers counseled me to disclose during follow-up visits, as a result, the child took responsibility for ARV drugs. In addition, when my child and I went to the hospital, the child asked me repeatedly questions why always we go to the hospital and take this drug but my friends do not take drugs for the reasons to disclose my child” (a caregiver of 10 years of old for a male child) and “Families have a responsibility to start the process of disclosure at home because they stay with the child for a long time. Children should be informed to increase adherence, relieve the stress of parents, prevent secondary transmission to others, prevent opportunistic infection, and have the right to know their disease status and to remind the caregivers of the appointments for follow-up” (Health care providers (HCP) from General Hospital).
Caregiver’s reasons for delaying disclosing HIV-positive status to infected children
Of the total caregivers of HIV-positive children who participated in the study, 161 (62.2%) did not disclose their HIV-positive status. As a result, caregivers stated the main reasons for delayed disclosure of the HIV-positive status of children. More than three-quarters of the caregivers (126 [78.3%]) of caregivers reported fear of their children’s refusal to take their drugs [Figure 3].
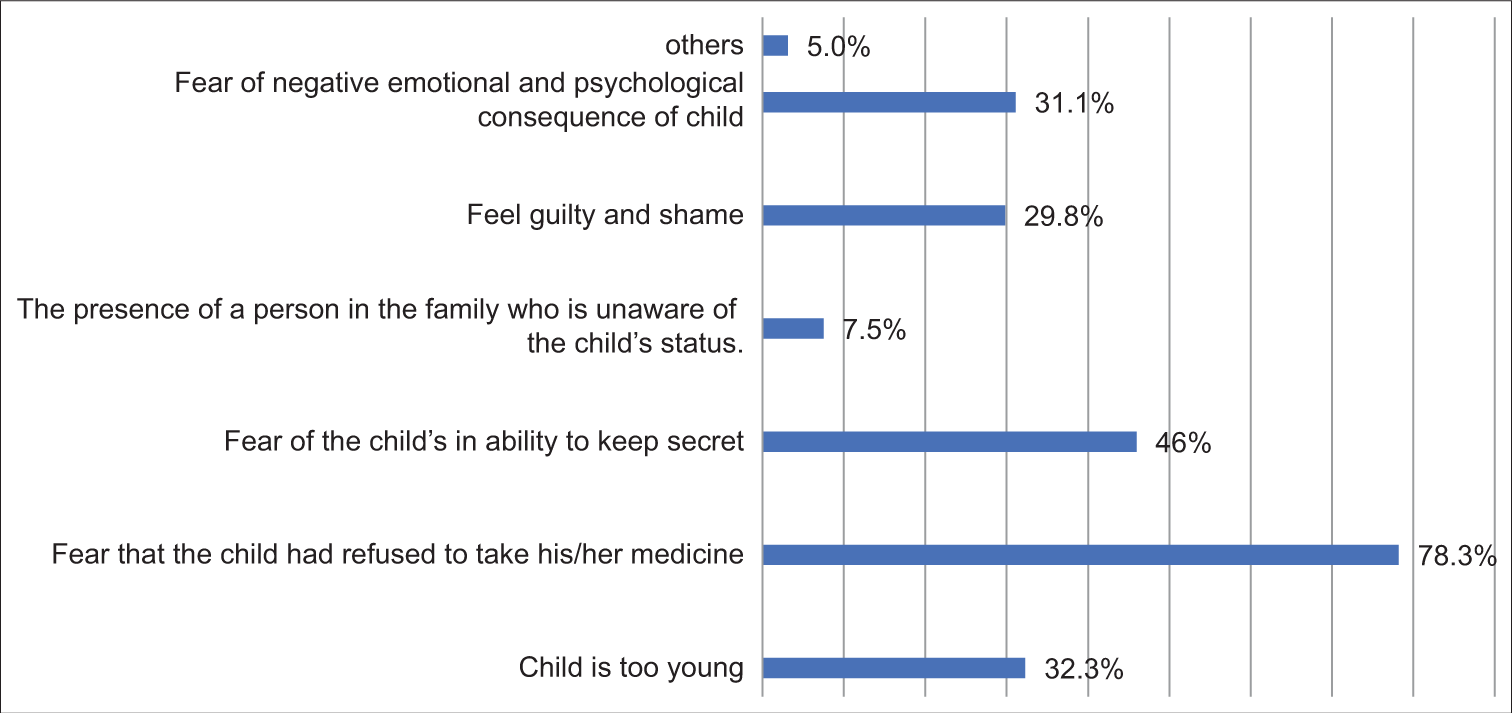
- Caregivers’ reasons for not disclosing HIV positive status to infected children in pediatric ART clinic at Gambella town public hospitals, Ethiopia, 2020(N=259). Others: Includes fear of stigma, discrimination and feel of hopelessness. Total percent exceeds 100% because multiple responses were possible.
The findings from the qualitative study were as follows; “I delayed disclosing my child’s HIV-positive status since he was too young to understand his illness, afraid that the child would keep secret because there was a person in the family who was not familiar with the status of the child and afraid of stigma and discrimination from friends and the community” (a caregiver of an 8-year-old male child). “There is no specific guideline for disclosure of HIV-positive children, as a result, it is difficult to counsel caregivers with their HIV-infected children. Additionally, caregivers believe that they are the cases for themselves and feel guilty and ashamed, because they believe that the child cannot understand the information and may disclose it to other people, resulting in stigma and discrimination from friends and the community” (HCP from Hospitals).
Factors associated with HIV-positive status disclosure to children
Binary logistic regression identified the following variables with P < 0.25 to be included in the final multivariable logistic regression model. These were the marital status of the caregiver, caregiver’s relation to a child, age of the child, educational level of the child, duration on ART of child, child’s responsibility of ARV drugs, child currently living with biological caregivers, WHO HIV clinical stage, and treatment adherence of child and caregivers’ HIV knowledge. Finally, four independent variables were found to be significantly associated with HIV-positive status disclosure to HIV-infected children P < 0.05 in the final model. These factors included the caregivers’ relationship with the child, the age of the child, duration of ART for the child, and recent ART treatment adherence for the child [Table 3].
| Variables | HIV status disclosure | Bivariate (COR [95%CI]) | Multivariate (AOR [95%CI]) | Multivariate- P-value | |
|---|---|---|---|---|---|
| Yes (n=98) | No (n=161) | ||||
| Caregivers’ relation to child | |||||
| Father | 30 (50.8) | 29 (49.2) | 4.66 (2.08, 10.44) | 5.37 (2.18, 13.21) | 0.000** |
| Mother | 56 (41.8) | 78 (58.2) | 3.23 (1.58, 6.60) | 3.65 (1.64, 8.15) | 0.002* |
| Grandparent and relatives | 12 (18.2) | 54 (81.8) | 1 | 1 | |
| Age of child (in years) | |||||
| <10 | 11 (13.6) | 70 (86.4) | 1 | 1 | |
| ≥10 | 87 (48.9) | 91 (51.1) | 6.08 (3.02, 12.26) | 3.73 (1.47, 9.49) | 0.006* |
| Duration on ART (in years) | |||||
| 1–5 | 18 (19.1) | 76 (80.9) | 1 | 1 | |
| 6–10 | 43 (40.2) | 64 (59.8) | 2.84 (1.49, 5.40) | 1.40 (0.60, 3.26) | 0.442 |
| 11–16 | 37 (63.8) | 21 (36.2) | 7.44 (3.54, 15.64) | 4.15 (1.56, 11.13) | 0.005* |
| Recent ART treatment adherence of child | |||||
| Good | 65 (47.4) | 72 (52.6) | 2.44 (1.45, 4.10) | 3.33 (1.81, 6.13) | 0.000** |
| Fair and poor | 33 (27.0) | 89 (73.0) | 1 | 1 | |
DISCUSSION
This study assessed the prevalence of HIV-positive status disclosure and its associated factors among children aged 6–18 years in two public hospitals, in Gambella town. The study showed that 37.8% (95% CI: 31.9%, 44.0%) of the HIV-positive children were positive for HIV. The result of this study is consistent with those of different studies conducted at Tikur Anbesa Specialized Hospital (32.4%), Hawassa Hospital (33.3%), North Gondar Hospital (39.5%), Malawi Hospital (36%), Tanzania Hospital (33%), and Latin America (39%).5,12,20,32-34 A possible explanation for the similarity with Tikur Anbesa Specialized Hospital might be the similar age groups of the children studied and the number of study participants, Hawassa is highly the similar to studied age group of children. In addition, similar to the study setting and in all the studies, additional information was collected from the caregivers of the HIV-positive children. The possible reasons for the results of studies performed in Malawi, Tanzania, and Latin America might be similar to those of the targeted studies of children in this population.
However, these percentages were greater than those in studies conducted in the Bale zone (28.5%), Addis Ababa (17.4%), Ghana (23%), and Nigeria (29.6%).9,21,25,31 The difference might be older age children included in this study, but Addis Ababa included all children age groups and in Bale zone, lower sample size and included 6–14-year-old children. In addition, a time difference and awareness might be created and different stakeholders may work in different areas to improve disclosure status. The differences between Ghana and Nigeria might be explained by sociocultural and health service differences.
However, these findings were lower than those of studies in Gondar town (44%), Dire Dawa (49.4%), Zimbabwe (67%), and Uganda (56%).13,23,24,28 The difference studies done in Gondar town and Dire Dawa might be the awareness of study participants toward disclosure of children, sample size differences and caregivers stated in this study and the child was too young to disclose and fear of the child’s refusal to take drugs and inability to keep secret. The differences between Zimbabwe and Uganda might be due to sociocultural differences such as stigma and discrimination related to HIV/AIDS and variation in the study setting. This is also supported by key informant interview findings; “Caregivers feel ashamed and guilty during disclosure, since they considered their children ask them the source of infection and might not keep secret” (HCP from hospitals).
Due to the remarkable improvements in providing access to pediatric HIV treatment, morbidity and mortality have been significantly reduced. As a result, CLWH survives into adolescence and adulthood; thus, HIV status disclosure is an essential element of pediatric HIV care and long-term disease management.35 In this study caregiver’s relationship with their child (biological father and mother), age 10 years and above, duration of ART (11–16 years), and recent ART adherence to the child (good) were associated with HIV-positive status disclosure.
Sixty-six (67.3%) children were informed about the study by their biological caregivers. Caregivers’ relationship with children was significantly associated with children’s HIV-positive status disclosure. Compared with grandparents and relatives, 5 biological fathers (AOR = 5.37; 95%CI: 2.18, 13.21) and 3.7 biological mothers (AOR = 3.65; 95%CI: 1.64, 8.15) were more likely to disclose their children’s HIV-positive status. However, these findings contradict those of North Gondar, which showed that non-biological caregivers were more likely to disclose than biological caregivers.12 A possible explanation for these differences might be the study period; the awareness of HIV-positive status disclosure by biological caregivers could be improved. As a result of this, biological caregivers might be eager to accept the responsibility for transmitting the infection to their children. However, in previous studies, caregivers were reluctant to disclose their children, since most children are infected by their HIV-infected mothers during pregnancy, childbirth, or breastfeeding.4,5 As a result, they are afraid and embarrassed about telling their children including that the child might hate them because they may be infected with the disease, fear parental guilt and shame, and fear that the children will not keep it secret.4,15,20 In addition, study period differences; counseling, and educating biological caregivers about disclosure by healthcare providers and other stakeholders might have gradually created better awareness and understanding of the benefits.
This is supported by key informant interviews; “child should be disclosed by his/her biological caregiver first then, discuss with health care provider since he/she knows the behavior of child and source of infection” (HCP from General Hospital). Thus, biological caregivers and health care providers should be responsible for disclosing the HIV-positive status of children to disclose their HIV-infected children.
Understanding the main reasons why caregivers delay disclosing their children’s HIV-positive status is important. The children were too young to understand and thought not mature because of caregivers’ reasons for not disclosing their status. However, this needs to be discussed with caregivers and age-appropriate disclosure should be provided based on the child’s cognitive development and emotional maturity.9 In this study, the age of the child was significantly associated with the child’s HIV-positive status disclosure. Children aged ≥10 years were 3.7 times (AOR = 3.73; 95% CI: 1.47, 9.59) more likely to be informed of their HIV-positive status by their caregivers than were children aged less than 10 years. This study is consistent with a study conducted in Gondar town, the Bale zone, Nigeria.24,25,31 A possible explanation for this similarity might be that caregivers perceived that older children inquired about their health conditions, and children thought that they could be able to understand the nature of the diagnosis and keep it secret. In this study, more than 80% of the children attended primary education, as a result, this might increase the likelihood of learning about HIV/AIDS. Moreover, 91.8% of the caregivers of disclosed children had good knowledge about HIV in the current study and this helps them to understand the benefit of disclosure. This is also supported by in-depth interviews; “I delayed disclosing my child since he is too young to understand the illness, fear stigma and discrimination, and the presence of the person in the family who is not familiar with the HIV status of the child” (caregiver of a 10-year-old female child). Disclosure at an early age might make children hopeless and prevent them from keeping secrets and understanding the nature of the virus.
According to the disclosure of their HIV-positive status, 81.6% of the children had spent at least 1 year on ART in this study. This finding is comparable with that of a study conducted in Gondar town (76%).24 The duration of ART was identified as an associated factor for HIV-positive status disclosure in children in this study. Children who were taking ART 11–16 years, 4 times (AOR = 4.15; 95%CI = 1.56, 11.13) were more likely to be aware of their HIV-positive status than children who were taking ART 1–5 years. These findings are consistent with studies conducted in Gondar town and the Bale Zone.24,31 The possible reasons for these similarities might be that children who stay on ART for a longer period are visited regularly and communicate with healthcare providers. As a result, caregivers and children receive continuing counseling which helps to facilitate disclosure, and no longer develop symptoms. Then, the children were asked their caregivers subsequent questions about their HIV drugs, and if this was not answered promptly, this may have led to decreased retention in care and refusal to take drugs. Therefore, the caregiver’s latter decision becomes to disclose her HIV status to the child. This is also supported by in-depth interviews; “a child asks me why I take this drug always long and when I stop this drug? but my school friend does not take drugs, mam, she said” (Caregiver of the 11-year-old female child). This finding suggested that a longer duration of ART might help children become aware of their health conditions.
There is a general expectation that following disclosure the child will be able to share his/her health conditions, help children understand the need for ART, and create trusting relationships that facilitate and improve adherence.23 A lack of knowledge is known to impact self-caretaking behavior and drug adherence. In this study, treatment adherence was significantly associated with children’s HIV-positive status disclosure. Compared with children who were not eligible for ART, those who had good ART treatment adherence were 3 times (AOR = 3.33; 95% CI: 1.81, 6.13) more likely to be disclosed by their caregivers. This finding is comparable to those of studies conducted in Tanzania and South Africa.5,36 A possible explanation might be that since the child is to stay on ART medication for the remainder of his/her life, caregivers believe that to improve treatment adherence, it is prudent to disclose the child’s status to him/her with the hope that the child will adhere to the treatment. In addition, children might refuse to take their ARV drugs and then, going to the clinic might wish to use disclosure as a means of facilitating better involvement by the child in treatment. This is supported by key informant interview findings; “Disclosure is important for the children and their caregivers since disclosing at appropriate age helps children to know their health conditions, take responsibility for their drugs and ask when health conditions are changed to their caregivers and health care providers” (HCP from hospitals). This finding suggested that disclosure affects improving treatment adherence in children.
This study produced rich information since the quantitative study was supplemented by qualitative methods of data collection. This study can be generalized to similar settings but not to the general population due to the facility-based nature of the study.
CONCLUSION
The prevalence of HIV positive status disclosure to infected children is lower in this study as compared to the studies performed in Gondar town and Dire Dawa. Caregiver’s relationship with the child (biological father and mother), age of the child, duration of ART, and adherence to ART treatment were associated with the disclosure of HIV-positive status to HIV-infected children. Therefore, ongoing counseling and health education for caregivers about disclosure and age appropriateness for children with cognitive development and working on related factors are important for improving low disclosure. Caregivers should discuss with healthcare providers HIV-positive status disclosure for their children, which should be repeated throughout the visit; this motivates them to disclose HIV-positive status to children at appropriate. In addition, performing further large-scale longitudinal studies is advisable to obtain a clear picture of the problem and its determinants in the country.
Acknowledgment
We thank Jimma University for financing this study, covering expenses for data collectors and other costs. We extend our gratitude to the Gambella Regional Health Bureau and Gambella town public hospitals for their cooperation during data collection at the study site. Special thanks also go to the caregivers of the HIV-positive children who participated in this study, for their willingness to share information about their children’s HIV status disclosure.
Ethical approval
The research/study was approved by the Ethical Review Board of the Institute of Health, Jimma University and a formal letter was obtained by Ref No. RB000104/2020 dated 9th March 2020.
Declaration of patient consent
Patients consent not required as the patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- The Global HIV/AIDS Epidemic In: Int Public Health (1st edition). 2018. p. :73-83.
- [CrossRef] [Google Scholar]
- HIV/AIDS in SubSaharan Africa: Current Status, Challenges and Prospects. Asian Pac J Trop Dis. 2017;7:239-56.
- [CrossRef] [Google Scholar]
- Disclosure of HIV Status to Children in Sub-Saharan Africa: A Systematic Review. Medicina (Kaunas). 2019;55:433.
- [CrossRef] [PubMed] [Google Scholar]
- Factors Associated with HIV Status Disclosure and Its Effect on Treatment Adherence and Quality of Life among Children 6-17 Years on Antiretroviral Therapy in Southern Highlands Zone, Tanzania: Unmatched Case Control Study. Int J Pediatr. 2018;2018:8058291.
- [CrossRef] [PubMed] [Google Scholar]
- HIV Related Estimates and Projections for Ethiopia-2017 Addis Ababa: The Ethiopian Public Health Institute; 2017.
- [Google Scholar]
- Disclosure of HIV Status to Children in Resource-limited Settings: A Systematic Review. J Int AIDS Soc. 2013;16:18466.
- [CrossRef] [PubMed] [Google Scholar]
- "Experiences with Disclosure of HIV-positive Status to the Infected Child": Perspectives of Healthcare Providers in Dar es Salaam, Tanzania. BMC Public Health. 2016;16:1083.
- [CrossRef] [PubMed] [Google Scholar]
- Factors Associated with HIV/AIDS Diagnostic Disclosure to HIV Infected Children Receiving HAART: A Multi-center Study in Addis Ababa, Ethiopia. PLoS One. 2011;6:e17572.
- [CrossRef] [PubMed] [Google Scholar]
- National Guideline for Comprehensive HIV Prevention. Care and Treatment. Ministry of Health. :137-46.
- [Google Scholar]
- Guideline on HIV Disclosure Counselling for Children up to 12 Years of Age Geneva: WHO; 2011.
- [Google Scholar]
- HIV-Positive Status Disclosure and Associated Factors among Children in North Gondar, Northwest Ethiopia. ISRN AIDS. 2012;2012:485720.
- [CrossRef] [PubMed] [Google Scholar]
- The Prevalence and Process of Pediatric HIV Disclosure: A Population-based Prospective Cohort Study in Zimbabwe. PLoS One. 2019;14:e0215659.
- [CrossRef] [PubMed] [Google Scholar]
- Perspectives and Practice of HIV Disclosure to Children and Adolescents by Health-Care Providers and Caregivers in sub-Saharan Africa: A Systematic Review. Front Public Health. 2016;4:166.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric HIV Disclosure in Northern India: Evaluation of Its Prevalence, Perceptions amongst Caregivers, and Its Impact on CLHIV. AIDS Res Treat. 2018;2018:2840467.
- [CrossRef] [PubMed] [Google Scholar]
- Socio-demographic, Clinical, and Psychosocial Factors Associated with Primary Caregivers' Decisions Regarding HIV Disclosure to Their Child Aged between 6 and 12 Years Living with HIV in Malawi. PLoS One. 2019;14:e0210781.
- [CrossRef] [PubMed] [Google Scholar]
- Disclosure of HIV Diagnosis to Infected Children Receiving Care in University of Uyo Teaching Hospital. J AIDS HIV Res. 2016;8:93-9.
- [CrossRef] [Google Scholar]
- A Model for HIV Disclosure of a Parent's and/or a Child's Illness. PeerJ. 2016;4:e1662.
- [CrossRef] [PubMed] [Google Scholar]
- Models of Support for Disclosure of HIV Status to HIV-infected Children and Adolescents in Resource-limited Settings. J Int AIDS Soc. 2018;21:e25157.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of disclosure of hiv positive status and its predictors among children and adolescents with hiv infection attending the paediatric infectious disease clinic at tikur anbessa specialized teaching hospital, addis ababa, ethiopia. . 2016;12:3-9.
- [Google Scholar]
- HIV Diagnosis Disclosure to Infected Children and Adolescents; Challenges of Family Caregivers in the Central Region of Ghana. BMC Pediatr. 2018;18:365.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants and Processes of HIV Status Disclosure to HIV--Infected Children Aged 4 to 17 Years Receiving HIV Care Services at Baylor College of Medicine Children's Foundation Tanzania, Centre of Excellence (COE) in Mbeya: A Cross-sectional Study. BMC Pediatr. 2015;15:81.
- [CrossRef] [PubMed] [Google Scholar]
- Factors Affecting Disclosure of Serostatus to Children Attending Jinja Hospital Paediatric HIV Clinic, Uganda. Afr Health Sci. 2015;15:344-51.
- [CrossRef] [PubMed] [Google Scholar]
- HIV Positive Status Disclosure and Associated Factor among HIV Infected Children in Pediatric ART Clinics in Gondar Town Public Health Facilities, North West Ethiopia, 2018. J Infect Public Health. 2019;12:873-7.
- [CrossRef] [PubMed] [Google Scholar]
- Disclosure of HIV Status to Infected Children and Adolescents by Their Parents/Caregivers in a Tertiary Health Facility in Abuja, Nigeria. Austin J HIV AIDS Res. 2018;5:1-7.
- [Google Scholar]
- Ethiopia Demographic and Health Survey 2016: HIV Report. In: Addis Ababa. Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2018.
- [Google Scholar]
- Challenges of Caregivers to Disclose their Children's HIV Positive Status Receiving Highly Active Anti Retroviral Therapy at Pediatric Anti Retroviral Therapy Clinics in Bahir Dar, North West Ethiopia. J AIDS Clin Res. 2013;4:11.
- [Google Scholar]
- Perinatally Acquired HIV-positive Status Disclosure and Associated Factors in Dire Dawa and Harar, Eastern Ethiopia: A Health Facility-based Cross-sectional Study. BMJ Open. 2018;8:e019554.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and Pattern of Disclosure of HIV Status in HIV-infected Children in Ghana. AIDS Behav. 2011;15:1121-7.
- [CrossRef] [PubMed] [Google Scholar]
- National Consolidated Guidelines for Comprehensive HIV Prevention. Care and Treatment.
- [Google Scholar]
- Human Immunodeficiency Virus Infection Disclosure Status to Infected School Aged Children and Associated Factors in Bale Zone, Southeast Ethiopia: Cross Sectional Study 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Pediatr. 2018;18:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Primary Caregivers, Healthcare Workers, Teachers and Community Leaders' Perceptions and Experiences of Their Involvement, Practice and Challenges of Disclosure of HIV Status to Children Living with HIV in Malawi: A Qualitative Study. BMC Public Health. 2018;18:884.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and Associated Characteristics of HIV-Infected Children in Latin America Who Know Their HIV Status. J Pediatric Infect Dis Soc. 2018;7:78-81.
- [CrossRef] [PubMed] [Google Scholar]
- Cross Sectional Characterization of Factors Associated with Pediatric HIV Status Disclosure in Southern Ethiopia. PLoS One. 2015;10:e0132691.
- [CrossRef] [PubMed] [Google Scholar]
- A cross-Sectional Study of Disclosure of HIV Status to Children and Adolescents in Western Kenya. PLoS One. 2014;9:e86616.
- [CrossRef] [PubMed] [Google Scholar]
- Disclosure of Human Immunodeficiency Virus Status to Children in South Africa: A Comprehensive Analysis. South Afr J HIV Med. 2019;20:884.
- [CrossRef] [PubMed] [Google Scholar]






