Translate this page into:
Exploring Barriers to Obstetric Care: A Case Report on High-Risk Pregnancy in a Limited-resource Primary Care Setting in West Bengal, India
*Corresponding author: Puspendu Biswas, Department of Community Medicine, Raiganj Government Medical College, Raiganj, West Bengal, India. puspendubiswas.commed@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Podder D, Mallick N, Dasgupta A, Biswas P. Exploring Barriers to Obstetric Care: A Case Report on High-Risk Pregnancy in a Limited-resource Primary Care Setting in West Bengal, India. J Compr Health. 2024;12:98-101. doi: 10.25259/JCH_14_2024
Abstract
Barriers to obstetric care have been under-researched in the Indian context, especially in limited-resource primary care settings. This case study seeks to unravel the barriers that lead to the high-risk pregnancy status of a 26-year-old second gravida, parity one pregnant mother residing in a rural area of West Bengal, India, in her 38 weeks of gestation with several risk factors. The factors that complicate the case include previous history of low birth weight delivery through cesarean section 4 years back, persistent anemia (Hemoglobin <10 g/dL), lately diagnosed hypothyroidism during the third trimester, and suboptimal weight gain of only 6 kg during the pregnancy (significantly below the recommended 9–11 kg gain) posing risks to both the mother and fetus. Ishikawa’s fishbone diagram has been used to illustrate the various categories and factors contributing to barriers to maternal care. Screening for risk factors, addressing the barriers, and timely case management and follow-up could improve fetomaternal health outcome.
Keywords
Barriers
High-risk pregnancy
Maternal care
Obstetric care
INTRODUCTION
High-risk pregnancies (HRPs) are a significant global public health concern, particularly in low-resource primary care settings. These pregnancies are fraught with increased risks of morbidity and mortality for both mother and child, necessitating early detection and effective management to mitigate adverse fetomaternal outcomes.1 The complexity of HRPs is underscored by myriad factors that can elevate pregnancy risk, including pre-existing medical conditions, complications arising during the perinatal period, and the sequelae of previous pregnancies. The Indian healthcare system has made strides in addressing these challenges through initiatives such as Pradhan Mantri Surakshit Matritva Abhiyan (PMSMA), Pradhan Mantri Matru Vandana Yojana, Janani Suraksha Yojana (JSY), and Janani Shishu Suraksha Karyakram which collectively provide a robust framework to support and manage HRPs by offering comprehensive maternal care.2 Despite such efforts, nearly 30% of pregnancies in India belong to high-risk groups, contributing to more than two-thirds of perinatal morbidity and mortality.3 This highlights the need to identify the gaps to effectively manage HRP cases, especially in limited-resource primary care settings in India.4
The case report highlights the challenges faced by a high-risk pregnant mother and potential barriers associated with managing such pregnancies in these settings, including limited access to specialized care and resources. By analyzing the factors contributing to this specific HRP, we aim to emphasize the importance of early detection, regular antenatal and postnatal care, and the need for collaborative efforts to improve maternal and fetal health outcomes.
CASE REPORT
This case study involves a 26-year-old high-risk pregnant mother with second gravida, parity one residing in a lower socioeconomic, five-membered joint family in a rural area of Uttar Dinajpur district of West Bengal, India. During a visit to her family, she was in her 38 weeks of gestation with several HRP-related risks, including previous history of low birth weight (LBW) delivery through cesarean section 4 years back, persistent anemia (hemoglobin [Hb] level <10 g/dL), lately diagnosed hypothyroidism during third trimester, and suboptimal weight gain of only 6 kg during the pregnancy (significantly below the recommended 9–11 kg gain).5
Data were collected through in-depth interviews in the local dialect (Bengali) at the participant’s residence and lasted for about 2 h. The interview followed a semi-structured guide, which included open-ended questions on personal background information, socioeconomic status, past experiences in accessing public health services, and family and community support toward family planning and pregnancy. A review of medical records related to current and past pregnancy was also made during the visit.
Obstetric history
The HRP woman has been married for 6 years, with her first pregnancy at 21 years of age, with no history of fetal loss (spontaneous or induced). She had a history of institutional delivery of an LBW, at term, a male child weighing 2.3 kg through lower segment cesarean section (LSCS) 4 years back. In her current pregnancy, she had a history of delayed recognition of pregnancy signs and pregnancy diagnosis. Antenatal registration at the local primary health center was made during the 14th week of gestation after the pregnancy was confirmed by an informal healthcare provider (HCP) using urine for a pregnancy test kit.
A review of medical records showed that the mother had visited the nearest block primary health center thrice for an antenatal checkup (ANC), where she was found to be normotensive, non-diabetic, and non-proteinuric throughout. However, she reportedly had signs of pallor with Hb level ranging from 7.6 g/dL during 1st ANC at 14 weeks gestation to 9.6 g/dL during 3rd ANC visit at 36 weeks of gestation. Her height was 155 cm, and she weighed 49.6 kg at the end of the third trimester. ANC history suggested that she had a suboptimal weight gain of only 6 kg during the pregnancy, whereas the ideal weight gain should range from 9 to 11 kg.5 Bilateral pitting edema was observed during her third ANC visit, and blood investigations revealed that she had hypothyroidism with low serum thyroxine and high thyroid-stimulating hormone value. Routine serologic tests for common blood-borne infectious diseases were found to be non-reactive. Other findings of blood tests are within normal limits. Ultrasonography findings at 36 weeks corroborated with the period of gestation and revealed a transverse lie of the fetus with anterior fundal placement of the placenta and adequate amniotic fluid.
The HRP was conservatively managed with daily iron folic supplementation prescribed for anemia prophylaxis and doses of tetanus-diphtheria vaccine as per guidelines. Following a diagnosis of hypothyroidism during the third trimester, levothyroxine supplementation in a dose of 75 mcg per day was prescribed. As evident from the mother and child protection (MCP) card, she was also counseled by the field-level primary HCP about birth preparedness, recognition of danger signs, optimum diet during pregnancy, and safe hygiene and sanitation practices.
Potential barriers
An in-depth interview and discussion with the mother revealed potential barriers that can be attributed to persistent anemia, lately diagnosed hypothyroidism during the third trimester, and suboptimal weight gain in the HRP woman with a previous history of LBW delivery through LSCS. Ishikawa fishbone diagram has been used to illustrate the various categories and factors contributing to barriers to obstetric care [Figure 1].
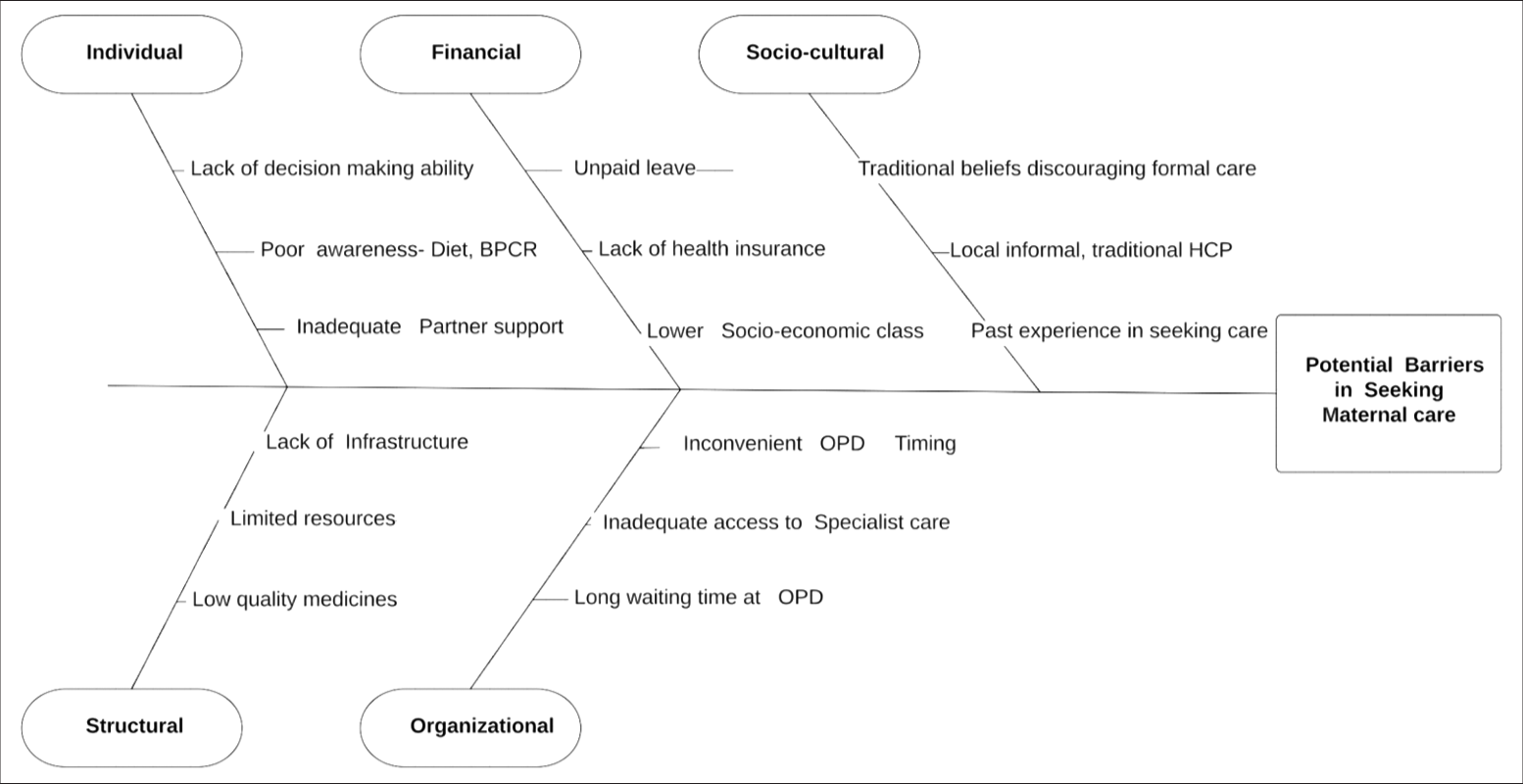
- Fish Bone diagram illustrating potential barriers to obstetric care in the high-risk pregnancy case; BPCR: Birth Preparedness and Complication Readiness, HCP: Health Care Provider, OPD: Out Patient Department.
DISCUSSION
HRPs account for nearly half of all pregnancies in India, with 33% of women having a single high-risk factor and 16.4% having multiple risks.1 Our case report delved into the intricacies of an HRP, examining the multifaceted barriers encountered by a woman as she navigates the complexities of seeking care within a limited-resource primary healthcare setting. This exploration sheds light on the critical need for systemic improvements to support and manage HRPs effectively, ensuring the health and safety of both mother and child. Existing maternal healthcare initiatives such as PMSMA and JSY need to be strengthened so that no mothers are left behind. It is to be ensured that every pregnancy-related risk is detected early and every woman receives at least four antenatal check-ups during her pregnancy. Collaborative efforts involving primary care providers [Accredited Social Health Activist (ASHA), Auxiliary Nurse and Midwife (ANM)], community physicians, and obstetricians are crucial in the timely identification and management of HRPs, such as those complicated by hypothyroidism, iron deficiency anemia, and malnutrition.6 Reportedly, in India, the prevalence of hypothyroidism in pregnancy ranges from 4.8 to 11.0%, of which the majority are subclinical and often are left untreated.7 Universal screening for hypothyroidism may be incorporated in the guidelines so that serious complications that may arise out of hypothyroidism- LBW, preterm birth, and cognitive and developmental disabilities in the child may be averted.8 Adhering to HRP management guidelines throughout the care continuum (e.g., mandating the use of a color-coded sticker system on the MCP card, even if there is a single risk factor that can lead to HRP status, timely follow-up, iron and folic acid (IFA) supplementation in therapeutic dosage, pre-identification of referral transport, and facility) may potentially improve fetomaternal health outcome. Addressing the family, community, and health system level barriers may further improve the quality of obstetric care provided.
CONCLUSION
Negative maternal and fetal outcomes can be significantly decreased by early detection and effective management of HRPs, thereby reducing maternal and perinatal mortality and morbidity. Capacity building of HCPs, addressing structural issues related to the workforce and supply chain along with focused educational intervention that is aimed to improve awareness among pregnant mothers, bring in positive change in their attitude, and enable them to seek formal care may be effective in realizing Sustainable Developmental Goal targets by 2030.
Acknowledgment
The authors would like to thank the participant and her family members for their voluntary participation and the field-level health workers for their cooperation in conducting this case study.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- High-risk Pregnancy in India: Prevalence and Contributing Risk Factors-A National Survey-based Analysis. J Glob Health. 2023;13:4116.
- [CrossRef] [PubMed] [Google Scholar]
- Pradhan Mantri Surakshit Matritva Abhiyan. Available from: https://pmsma.mohfw.gov.in [Last accessed on 2024 Feb 12]
- [Google Scholar]
- High Risk Pregnancy. Available from: https://www.nhp.gov.in/disease/gynaecology-and-obstetrics/high-risk-pregnancy [Last accessed on 2024 Jan 24]
- [Google Scholar]
- A Longitudinal Study on High Risk Pregnancy and Its Outcome among Antenatal Women Attending Rural Primary Health Centre in Puducherry, South India. J Educ Health Promot. 2019;8:12.
- [CrossRef] [PubMed] [Google Scholar]
- Park's Textbook of Preventive and Social Medicine (27th ed). India: Banarsidas Bhanot Publishers; 2023.
- [Google Scholar]
- Nurturing Inter-professional Collaboration for Positive Childbirth Experiences. J Taibah Univ Med Sci. 2023;18:842-3.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Hypothyroidism in Pregnancy: An Epidemiological Study from 11 Cities in 9 States of India. Indian J Endocrinol Metab. 2016;20:387-90.
- [CrossRef] [PubMed] [Google Scholar]
- Clinico-epidemiological Profile of Women with High-risk Pregnancy Utilizing Antenatal Services in a Rural Primary Health Center in India. J Rural Med. 2023;18:15-20.
- [CrossRef] [PubMed] [Google Scholar]