Translate this page into:
COPD, Asthma and Pneumothorax as Climate Sensitive Health outcomes
Corresponding author: Dr. Mathew J Valamparampil, Senior Resident, Community Medicine, Government Medical College Hospital, Trivandrum, Kerala, India. Email: mathewivalamparampil@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Insija IS, Dennis PJ. Jemin AJ, Valamparampil MJ, Pillai HKG, Gayatri Bindu Nair GB et al. COPD, Asthma and Pneumothorax as Climate Sensitive Health outcomes. J Comprehensive Health.2018; 6(2):82-89
Abstract
Background:
Chronic Obstructive Pulmonary Disease(COPD), pneumothorax and asthma are climate sensitive diseases contributing a significant proportion of the respiratory disease morbidity. Even when the monsoon rainfall is high, recent years have witnessed an increase in the average temperature in Kerala. The study aims to determine the trends in hospital admissions for these diseases and associated factors during 2011 to 2015 at a tertiary care hospital in Thiruvananthapuram, India.
Methods:
Record based retrospective study was done at Chest Disease Hospital at Thiruvananthapuram, Kerala. Data regarding the patients admitted from January 2011 to December 2015 was collected and trend analysis was done. Change in occurrence over the 5 year period was estimated and associations with co-existing diseases were determined.
Results:
A significant difference in the occurrence of COPD cases was seen during the months of July to December when compared between 2011 and 2015 with a significant rise in mean age of occurrence(p<0.001). Similar findings was seen with asthma with seasonally varying occurrences resulting in increased hospital admissions. No such seasonal variation could be seen for pneumothorax.
Conclusions:
The consistently shifting age patterns and the seasonal variation in occurrences, are in line with evidences from around the world which points to the urgent focus to be given to climate related respiratory diseases. Steady increase in occurrence of asthma and significant association of COPD with several co-morbidities are important areas of concern.
Keywords
Chronic Obstructive Pulmonary Disease
Asthma
Pneumothorax
Climate
Introduction
Climate is defined as the sum of atmospheric elements and the variations occurring in them through the main meteorological parameters like solar radiation, temperature, humidity, clouds, wind and atmospheric pressure. Climate change refers to any change in climate over time, whether due to natural variability or as a result of human activity. Climate change is an environmental issue as well as a grave health issue. As communicable diseases like tuberculosis and non-communicable diseases like diabetes and hypertension continue to plague developing countries like India, the significant differences in their occurrence in association with climate sensitive outcomes should be viewed with utmost caution. This is because the changes in climatic scenario negatively affects these countries, especially their poorest.
The effects of climate change and global warming on human health, in particular in patients with lung disease, are poorly understood at present. The lungs are in direct contact with the environment and are a sort of portal organ of climate change. Climate change is not only having an impact on air pollution but also on distribution and quality of aero-allergens and the dissemination and transmission of respiratory pathogens.
Chronic Obstructive Pulmonary Disease (COPD), pneumothorax and asthma are the respiratory diseases considered as climate sensitive. These three diseases contribute a significant proportion of the respiratory morbidity. Excessive cold temperatures have been linked to increases in mortality and morbidity in individuals affected with COPD. COPD response to cold temperature includes bronchoconstriction, inflammation and mucous hypersecretion.
Weather influences asthma directly by acting on airways or indirectly, by influencing airborne allergens and pollutant levels.- Decrease in air temperature represents an aggravating factor of asthmatic symptoms, regardless of geo-climatic variations. It causes respiratory symptoms that are interspersed with severe attacks, which may require urgent health care and may be fatal. Indian asthmatics have a high frequency of reported exacerbations (67%), leading to substantial functional and emotional limitations.
Asthma and COPD were typically characterized as different diseases with unique epidemiological features as well as pathophysiological mechanisms. However, this concept needs to be re-evaluated as many epidemiological studies have shown that asthma and COPD may coexist, or at least one condition may evolve into the other creating a condition commonly described as Asthma and COPD Overlap Syndrome(ACOS). They are known to experience more frequent exacerbations, poorer quality of life, usually a more rapid decline in lung function, and higher morbidity and mortality than those with either COPD or asthma alone, not unlike what is observed with other comorbidities.
Pneumothorax is the presence of gas in the pleural space. A spontaneous pneumothorax is the one that occurs without antecedent trauma to the thorax. A primary spontaneous pneumothorax (PSP) occurs in the absence of underlying lung disease, whereas a secondary pneumothorax occurs in its presence. Most secondary pneumothoraxes are due to chronic obstructive pulmonary disease (COPD), but pneumothoraxes have been reported with virtually every lung disease. Pneumothorax in patients with lung disease is more life-threatening than it is in normal individuals because of the lack of pulmonary reserve in these patients.
Climate Scenario In Kerala
Kerala is the land of monsoons. It is also one of the wettest places in the world, where annual rainfall is of the order of 3000mm. About 68 per cent of the rainfall is obtained during southwest monsoon while 16 per cent in post monsoon and the rest from summer (14%) and winter rainfall (2%).
A clear upward trend in surface air temperature across the West Coast between 1961 and 2003 by 0.8°C in maximum and 0.2°C in minimum temperature with an increase in average surface air temperature of 0.6°C was noticed. According to India Meteorological Department (IMD), during the last 43 years, the mean maximum temperature over Kerala has risen by 0.8°C, the minimum by 0.2°C and the average by 0.5°C, indicating that the temperature trends in Kerala followed the trends of West Coast. February and March are the hot months of Kerala with a mean maximum of 33°C.
This study aimed at looking at trends in hospital admissions for three climate sensitive respiratory illnesses namely COPD, Asthma and Pneumothorax during the period 2011 to 2015 in Chest Disease Hospital, Thiruvananthapuram Kerala. We also examined the differences in age, gender and co-existing morbidities in 2015 as compared to the base year 2011.
Material & Methods
As a part of development of a Climate Resilient Health Sector in Kerala India, an expert committee was created for the state of Kerala which identified the above three diseases as important health indicators for changing patterns in climate. The study was conducted under the guidance of the expert panel to determine the trends in the occurrence of these diseases along with the overall difference in occurrence between 2011 and 2015. The study was a record based retrospective study in which the details of patients were obtained from records at Chest Disease Hospital Pulayanarkotta, Thiruvananthapuram Kerala. This is the pulmonary care division of Government Medical College Thiruvananthapuram which predominantly caters to the population of Thiruvananthapuram and Kollam districts of Kerala. The data regarding the patients admitted from January 2011 to December 2015 was collected from ward registers and trend analysis was done using the cumulative annual figures. The age, gender and co-existing morbidities of patients admitted with COPD, asthma and pneumothorax during 2011 and 2015 were also collected. It was analyzed to look for any changes, over the five year period. As the study was conceived as a record based operational research venture, it was exempted from obtaining ethical clearance by the government.
Results
The number of patients diagnosed with asthma gradually increased over the five years. An increase in total number of cases was seen in the case of pneumothorax also. There was not much change in the cumulative total of patients diagnosed with COPD over the 5 year period.(Table 1).
| COPD | Asthma | Pneumothorax | |
|---|---|---|---|
| 2011 | 1440 | 370 | 88 |
| 2012 | 1335 | 482 | 96 |
| 2013 | 1151 | 378 | 104 |
| 2014 | 1384 | 489 | 101 |
| 2015 | 1328 | 619 | 125 |
COPD
According to our study there was an increase in mean age of patients admitted with COPD; 62.87 (SD-9.97) and 64.29 (SD-9.18) in 2011 and 2015 respectively. This rise in mean age was also seen to have statistical significance (p < .001). The number of patients admitted due to COPD in the year 2011 was 1440 and in 2015 was 1332.(Table 1) A higher proportion of COPD patients were males during both years (84.5 and 75.0% respectively). There is a significant reduction in the proportion of affected males in 2015 compared to 2011(p < .001). The month-wise and year-wise variation in the number of cases has been shown in Figure 1. Each quarter-year(3 months) of 2011 was compared with the corresponding quarter-year of 2015. The number of cases decreased from 355 to 282 in the period of July to September of 2011 & 2015. There was still further increase from 332 to 351 in the period of October to December between the two years.(48.6% to 51.4%). Also, each quarter-year was compared with the rest of the 9 months in 2015. The occurrence of cases in both the quarter-years were found to be proportionately more, when compared with the rest of the 9 months in 2015.(Table 2)
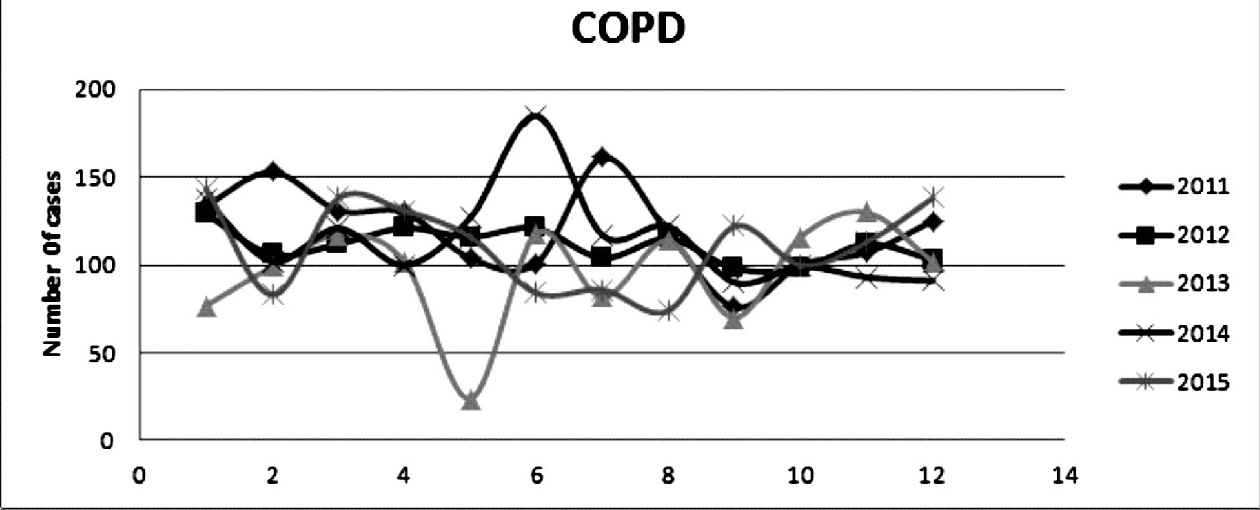
- Trend of patients admitted with COPD 2011 - 2015
| 2011 | 2015 | ||
|---|---|---|---|
| COPD | July-September | 355(24.65%) | 282(21.17%) |
| Rest 9 months | 1085(75.35%) | 1050(78.83%) | |
| COPD | October-December | 332(23.1%) | 351(26.4%) |
| Rest 9 months | 1108(76.9%) | 977(73.6%) | |
| Asthma | July-September | 90(24.3%) | 114(18.4%) |
| Rest 9 months | 280(75.7%) | 506(81.6%) | |
| Asthma | October-December | 83(22.4%) | 188(30.4%) |
| Rest 9 months | 287(77.6%) | 431(69.6%) |
The present study has found an increase in occurrence of other co-morbidities. Compared to 2011, in 2015 the occurrence of diabetes mellitus (4.6% to 7.4%), hypertension (3.4% to 7.3%) and coronary artery disease (0.8% to 3.5%) increased among COPD patients. Similarly, history of tuberculosis infection among COPD patients has also significantly increased in 2015 (6.8% to 10.1%). The proportion of patients who had prior history of treatment with Anti-tubercular therapy (ATT) sharply increased from 6.7% to 9.6% while those who were presently on ATT increased from 0.1% to 0.5%.
Among the patients admitted with COPD, there an increase in proportion of those suffering from bronchiectasis (1.9% to 4.4%) in 2015 as compared to 2011. Similarly a rising trend (1.3 to 2.9%) for COPD associated pneumothorax was also seen. The number of patients with COPD with co-existing pneumothorax doubled from 15 to 30 between 2011 and 2015 while those suffering from hydro pneumothorax increased from two to seven. Significant increase was seen in the case of associated corpulmonale also (1.9% to 4.3%).
Of the patients diagnosed with COPD, only 0.8% had co existing bronchial asthma in 2011 while it rose to 7.4% in 2015. Due to differences in diagnostic criteria, patients with COPD were not diagnosed as having ACOS in 2011 while one was diagnosed as having ACOS in 2015. The results of analysis with regards to COPD are given in Table 3.
| 2011 | 2015 | ||
|---|---|---|---|
| Asthma | present | 11 (.8%) | 98 (7.4%) |
| absent | 1429(99.2%) | 1234(92.6%) | |
| Pneumonia | present | 12 (.8%) | 9 (.7%) |
| absent | 1428(99.2%) | 1323(99.3%) | |
| ACOS | present | 0 | 1(.1%) |
| absent | 1440(100%) | 1331(99.9%) | |
| Diabetes | present | 66(4.6%) | 98(7.4%) |
| absent | 1374 | 1234 | |
| Hyper tension | present | 49(3.4%) | 97(7.3%) |
| absent | 1391 | 1235 | |
| CAD | present | 12(.8%) | 47(3.5%) |
| absent | 1428 | 1285 | |
| CorPulmonale | present | 27(1.9%) | 57(4.3%) |
| absent | 1413 | 1275 | |
| Bronchiectasis | present | 28(1.9%) | 58(4.4%) |
| absent | 1412 | 1274 | |
| Pneumothorax | Present | 18(1.3%) | 30(2.9%) |
| Absent | 1422(98.7%) | 1294(97.1%) | |
| Tuberculosis infection | Present | 98(6.8%) | 134(10.1%) |
| Absent | 1342(93.2%) | 1198(89.9%) |
Asthma
The number of patients admitted due to asthma in the year 2011 was 370 and in 2015 was 620.(Table 1) A higher proportion of patients were females during both years (75.9% and 85.5% respectively) with a significant increase in 2015 compared to 2011(p < 0.001). The results of analysis with regards to Asthma are given in Table 4. A similar increase(p <0.001) in mean(SD) age of patients admitted with asthma was also seen; 49.81(14.39) to 53.39(14.03) years.
| 2011 | 2015 | ||
|---|---|---|---|
| COPD | present | 11(3%) | 98(15.8%) |
| absent | 359(97%) | 522(84.2%) | |
| Pneumonia | Present | 5(1.4%) | 0 |
| absent | 365(98.6) | 620(100%) | |
| ACOS | present | 0 | 0 |
| a bsent | 370 | 620 | |
| Diabetes | present | 33(8.9%) | 38(6.1%) |
| a bsent | 337(91.1%) | 582(93.9%) | |
| Hyper tension | present | 35(9.5%) | 35(5.6%) |
| absent | 335(90.5%) | 585(94.4%) | |
| CAD | present | 4(1.1%) | 6(1%) |
| absent | 366(98.9%) | 614(99%) | |
| CorPulmonale | present | 3(0.8%) | 6(1%) |
| absent | 367(99.2%) | 614(99%) | |
| Bronchiectasis | present | 9(2.4%) | 20(3.2%) |
| absent | 361(97.6%) | 600(96.8%) | |
| Pneumothorax | Present | 0 | 4(0.6%) |
| Absent | 370 | 616(99.4%) | |
| Treatment for Tuberculosis | Present | 7 (1.9%) | 9(1.5%) |
| Absent | 363 (98.1%) | 611(98.5%) |
*Chi-square test is used
+p value less than 0.05 is considered as statistically significant
Increased occurrence could be seen in the colder months with a similar trend beingh visualized in all the years.(Figure 2) A significant difference between the occurrences of cases was found between the 2nd half of 2011 and 2015. The number of cases increased from 90 to 114 in the period of July to September of 2011 & 2015. There was still further increase from 83 to 188 in the period of October to December between the two years. The occurrence of cases in both these quarters were found to be higher when compared with the rest of the year. (Table 2)
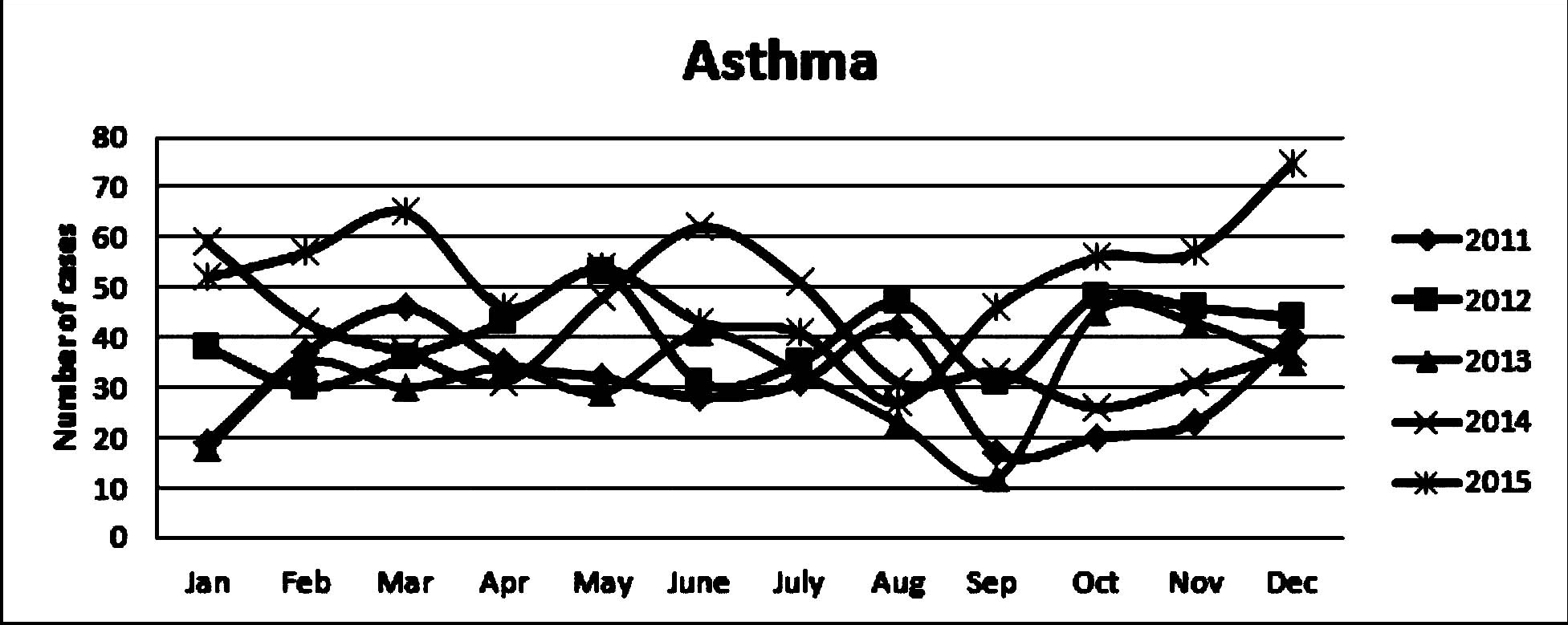
- Trend of patients admitted with Asthma 2011 - 2015
Similarly, in those diagnosed with asthma, a co-existing COPD was seen only in 3% in 2011 which rose to 15.8% in 2015. Co- morbidities like diabetes mellitus (8.9% to 6.1%), and history of tuberculosis infection (1.9% to 1.5%) were also found to be lower in 2015. Patients who had prior history of treatment with Anti-tubercular therapy (ATT) remained almost constant at 1.9% and 1.5% between both years. But a significant decrease in hypertension (9.5% to 5.6%) among patients affected with asthma was seen.
Pneumothorax
In the year 2011, 88 patients got admitted with pneumothorax which increased to 125 in 2015.(Table 1) The mean(SD) age of occurrence increased from 48.92(18.36) to 54.24(15.34) years. The proportion of males among them increased from 78.4% to 88.1%. In our study the male-female ratio in patients admitted with secondary pneumothorax was 3.63:1 in 2011, which increased to 7.4:1 in 2015. The results of analysis with regards to COPD are given in Table 5.
There was no month-wise or quarter-wise difference in the occurrence of the disease as the number of cases were found to be similar in all months of both years with a general increase in 2015.(Figure 3) But, there was a sharp rise of 20.5% to 30.2% in the proportion of patients suffering from coexisting COPD (18 patients in 2011 and 38 in 2015).
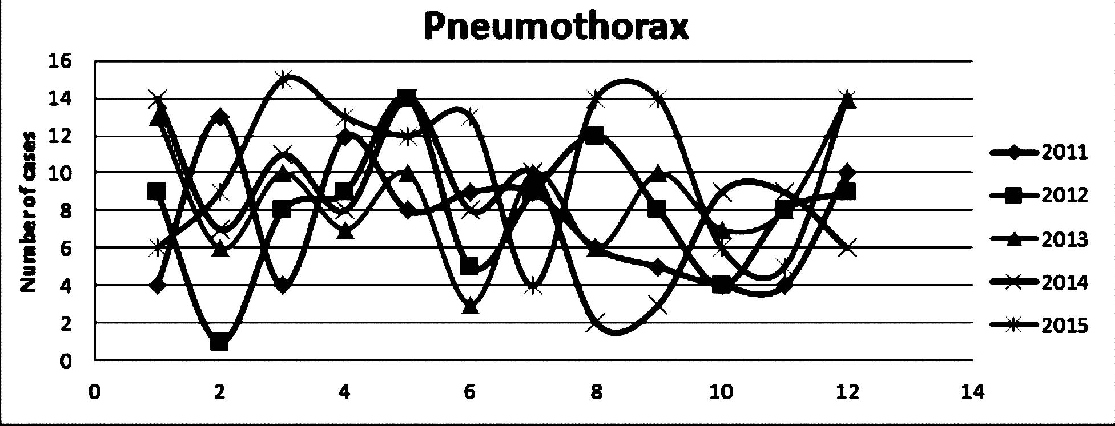
- Trend of patients admitted with Pneumothorax 2011 - 2015
Also, occurrence of other co-morbidities were found to be minimal and history of tuberculosis treatment was similar when compared between 2011 and 2015.
Discussion
COPD
The increased episodes of COPD during the winter season due to the role of lower temperature and suspended particulate matter have been shown in studies conducted in Delhi. It is also consistent with the findings of increased exacerbations detected in studies conducted in the United Kingdom. Even though excessive cold temperatures have been linked to increases in mortality and morbidity in individuals affected with COPD,[16] the findings from this study should be used for creating increasing awareness about the role of seasons in disease patterns even in Kerala where the seasonal fluctuations are not as drastic as seen elsewhere. About 97 % of COPD patients has atleast one comorbidity with an average of four comorbidities per patient; the most frequent being cardiovascular disease(69%) which also contributes to mortality of the patient. Studies have demonstrated the association between COPD and type 2 diabetes. With increasing awareness on the role inflammatory components play in both COPD and T2DM, the inflammatory process in each disease and the potential interplay between them are considered as very important pathogenesis of both diseases. Similar to this study, systemic arterial hypertension has been described as a major comorbidity associated with COPD, as demonstrated by a population-based case-control study conducted in Switzerland, Korea, Japan and many other countries. High blood pressure might be associated with reduced lung function in a general adult population. Chronic hypertension causes left ventricular dysfunction, which again results in elevated left atrial pressure. This in turn can lead to an elevation of pulmonary artery pressure, an increase in interstitial edema in the lung and hence causing a fall in lung compliance and functional residual capacity, resulting in decreased FEV1 and FVC values.
The present study as well as previous studies showed a high rate of coexistence of bronchiectasis and COPD. Global Initiative for Chronic Obstructive Lung Disease (GOLD) describes bronchiectasis as an important comorbidity of COPD. They share common characteristics in clinical presentations and pathophysiology such as chronic cough, sputum production, susceptibility to recurrent exacerbations and incompletely reversible airflow obstruction.' Similarly, the association of tuberculosis with the FEV1/FVC ratio were seen to be characterized by an obstructive pattern.
Asthma
Increased occurrence asthma with seasonal variations has been reported in India as was seen in the present study. The total number of cases have increased substantially in 2015 when compared to 2011 along with a similar increase in proportion of females. This finding is in line with the evidences pointing to the shift from males to females with advancing age. The changes in occurrence of asthma in line with the seasonal variations is similar to those seen in COPD. Seasonal variations in asthma related hospital admissions, its relation with presence of aero-allergens etc have been demonstrated. Here, both the third and final quarters of the year was found to be different from the rest of the year in terms of occurrence of disease. But this can vary slightly from place to place. Each geographical region will have its own unique climatic and environmental factors which can thus contribute to varying occurrences of disease patterns in the region.
The gender-switch happens at puberty (the exact age based mostly on cross-sectional data reports from 11 to 18 years of age) causing increased female prevalence. Similarly, in those diagnosed with asthma, a co-existing COPD was seen only in 3% in 2011 which rose to 15.8% in 2015.
Pneumothorax
The number of patients admitted with pneumothorax showed a slight increase over the years. The mean age of occurrence after 40 years of age is similar to previous findings. The increase in male-female ratio in patients admitted with secondary pneumothorax from 3.63:1 to 7.4:1 is similar to the findings seen in a study conducted in Thailand having male to female ratios of 7.5:1 and 4.1:1 for primary and secondary spontaneous pneumothorax respectively. Similarly, the absence of month wise or quarter wise difference in the occurrence of the disease in this study was similar to earlier studies in which emergency admissions for pneumothorax was not linked to specific monthly, seasonal or annual periodicities. While COPD has been stated as the predominant cause of SSP in developed countries, tuberculosis has remained as the dominant cause in India. Hence a lack of difference in occurrence with respect to seasons could be explained from the present study.
Strengths and Limitations
This study is one among the first attempts to link respiratory diseases with climatic change in Kerala. The preciseness of the records regarding hospital admissions has helped in making valid associations and conclusions. As the total number of people admitted at the hospital is not known, no comments could be made about the changing proportion of each disease.
Conclusion and recommendations
The steady increase in the occurrence of bronchial asthma and the significant association of COPD with many co-morbidities are important areas of concern. The shifting age patterns and the seasonal variation in occurrences are consistently present. Similarity of these findings with evidences from around the world, points to the urgent focus to be given to climate related changes in health. The differences seen cannot be attributed to climate variations alone due to lack of data on climate related variables specifically pertaining to Kerala. The health system should be equipped to capture this data in order to intervene effectively in reducing vulnerabilities and improve adaptations of people with respiratory morbidities.
Conflict of Interest:
None declared
Source of support:
Nil
References
- Weather Underground [Internet] Available from: https://www.wunderground.com/resources/climate/ipcc2007.asp (accessed )
- [Google Scholar]
- World Bank Available from: http://www.worldbank.org/en/news/feature/2014/03/03/climate-change-affects-poorest-developing-countries (accessed )
- IMPACTS, VULNERABILITIES AND ADAPTATION IN DEVELOPING COUNTRIES - impacts.pdf. Available from: http://unfccc.int/resource/docs/publications/impacts.pdf (accessed )
- [Google Scholar]
- Heat stress in older individuals and patients with common chronic diseases. CMAJ Can Med Assoc J J Assoc Medicale Can. 2010;182(10):1053-60.
- [CrossRef] [PubMed] [Google Scholar]
- [The effects of air pollution and climate change on pulmonary diseases] Dtsch Med Wochenschr 1946. 2008;133(14):733-6.
- [CrossRef] [PubMed] [Google Scholar]
- The Effects of Air Pollution and Temperature on COPD. COPD. 2016;13(3):372-9.
- [CrossRef] [PubMed] [Google Scholar]
- Bronchoconstriction due to cold weather in COPD. The roles of direct airway effects and cutaneous reflex mechanisms. Chest. 1996;110(3):632-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cold temperature induces mucin hypersecretion from normal human bronchial epithelial cells in vitro through a transient receptor potential melastatin 8 (TRPM8)- mediated mechanism. J Allergy Clin Immunol. 2011;128(3):626-634. e1-5
- [CrossRef] [PubMed] [Google Scholar]
- Assessing respiratory morbidity through pollution status and meteorological conditions for Delhi. Environ Monit Assess. 2006;114(1-3):489-504.
- [CrossRef] [PubMed] [Google Scholar]
- Outdoor air pollution and emergency room visits at a hospital in Delhi. Indian J Chest Dis Allied Sci. 2002;44(1):13-9.
- [Google Scholar]
- Seasonal Variation of Allergenic Acarofauna From the Homes of Allergic Rhinitis and Asthmatic Patients. J Med Entomol. 2018;55(2):262-8.
- [CrossRef] [PubMed] [Google Scholar]
- Meteorological parameters and pollutants on asthma exacerbation in Bangalore, India - an ecological retrospective time-series study. J Basic Clin Physiol Pharmacol. 2017;28(2):133-41.
- [CrossRef] [PubMed] [Google Scholar]
- Insights, attitudes and perceptions about asthma and its treatment: findings from a multinational survey of patients from 8 Asia-Pacific countries and Hong Kong. Respirol Carlton Vic. 2013;18(6):957-67.
- [CrossRef] [PubMed] [Google Scholar]
- Asthma and COPD Overlap Syndrome (ACOS): A Systematic Review and Meta Analysis. PloS One. 2015;10(9):e0136065.
- [CrossRef] [PubMed] [Google Scholar]
- The asthma-COPD overlap syndrome: how is it defined and what are its clinical implications? J Asthma Allergy. 2016;9:27-35.
- [CrossRef] [PubMed] [Google Scholar]
- State Level Climate Change Trends in India Meteorological Monograph No. ESSO/IMD/EMRC/02/2013 [Internet] India Meteorological Department, Ministry of Earth Sciences, government of India 2013 Available from: http://www.imd.gov.in/pages/ services_climate.php?adta=PDF&adtb=&adtc=../section/climate/StateLevelClimateChangeMonoFinal (accessed )
- [Google Scholar]
- The causes and consequences of seasonal variation in COPD exacerbations. Int J Chron Obstruct Pulmon Dis. 2014;9:1101-10.
- [CrossRef] [PubMed] [Google Scholar]
- Association of chronic obstructive pulmonary disease with type 2 diabetes mellitus. Chin Med J (Engl). 2014;127(17):3185-6.
- [CrossRef] [Google Scholar]
- Prevalence of chronic obstructive pulmonary disease among patients with systemic arterial hypertension without respiratory symptoms. Int J Chron Obstruct Pulmon Dis. 2015;10:1525-9.
- [CrossRef] [PubMed] [Google Scholar]
- Association between lung function, hypertension and blood pressure medication. Respir Med. 2011;105(5):727-33.
- [CrossRef] [PubMed] [Google Scholar]
- Co-morbidities in patients with gold stage 4 chronic obstructive pulmonary disease. Rev Port Pneumol. 2014;20(1):5-11.
- [CrossRef] [Google Scholar]
- Chronic obstructive pulmonary disease and bronchiectasis. Curr Opin Pulm Med. 2013;19(2):133-9.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical characteristics of patients with chronic obstructive pulmonary disease with comorbid bronchiectasis: a systemic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2015;10:1465-75.
- [CrossRef] [PubMed] [Google Scholar]
- Global Initiative for Chronic Obstructive Lung Disease - GOLD. Available from: http://goldcopd.org/ (accessed )
- [Google Scholar]
- Climatic conditions and the onset of primary spontaneous pneumothorax: an investigation of the influence of solar terms. Med Princ Pract Int J Kuwait Univ Health Sci Cent. 2012;21(4):345-9.
- [CrossRef] [PubMed] [Google Scholar]
- Social and familial factors in the development of early childhood asthma. Pediatrics. 1985;75(5):859-68.
- [CrossRef] [PubMed] [Google Scholar]
- Gender differences in prevalence, diagnosis and incidence of allergic and non-allergic asthma: a population-based cohort. Thorax. 2012;67(7):625-31.
- [CrossRef] [PubMed] [Google Scholar]
- Associations between pollen counts, pollutants, and asthma-related hospital admissions in a high-density Indian metropolis. J Asthma Off J Assoc Care Asthma. 2012;49(8):792-9.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship of sex to asthma prevalence, health care utilization, and medications in a large managed care organization. Ann Allergy Asthma Immunol Off Publ Am Coll Allergy Asthma Immunol (6):553-8.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of spontaneous pneumothorax in adults in a tertiary care hospital. Lung India Off Organ Indian Chest Soc. 2015;32(4):415-6.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence, clinical manifestations and mortality rate in patients with spontaneous pneumothorax in Thammasat University Hospital. J Med Assoc Thail Chotmaihet Thangphaet. 2013;96(10):1290-7.
- [Google Scholar]






