Translate this page into:
Assessment of Nutritional Status of Under-5 Children in A Slum of Kolkata, West Bengal: A Community Based Study
Corresponding Author : Dr. Tania Pan Address - All India Institute of Hygiene and Public Health,110 C R Avenue, Kolkata Phone number-7980366722, E-mail address-taniapanl902@gmail.com
Abstract
Background:
The nutritional status of under-5 children in slums is an important health indicator for assessing the health status of entire population. Reduction in malnutrition is a Millennium Development Goal (MDG) to improve child welfare. The study was conducted to assess the nutritional status of under-5 children in a slum of Kolkata and its associated factors.
Materials and Methods:
It was an observational, cross-sectional study among under-5 children in a slum area of Kolkata, West Bengal, India to determine nutritional status and its determinants using WHO Z-score and Composite Index of Anthropometric Failure (CIAF). A total of 129 under-5 children were included by simple random sampling. Data entry was done in SPSS. All ethical issues were addressed.
Results:
Out of total 129 children assessed, 31.8% were found to have anthropometric failure using CIAF. However, with standard anthropometric indices such as weight-for-age, weight-for-height, height-for-age, and mid upper arm circumference,17.8% were underweight, 9.3% were wasted, 16.3% were stunted and 14% were undernourished respectively. About 40.3% children had morbidity within last 2 weeks (acute respiratory infection 25.6%, diarrhoea 3.9%, fever 10.9%). Literacy of mother [AOR-3.79 (1.39-10.33)], exclusive breast feeding [AOR- 6.1 (1.80-8.79)], personal hygienic practice [AOR-3.17 (1.02-10.02)] and morbidity profile [AOR-2.95 (1.13-7.72)] were significantly associated with nutritional status.
Conclusion:
The study identifies maternal education and care and infant and child feeding practices to have a bearing on the nutritional status of the children. Further large scale studies are warranted to determine the alleviation in the situation afteraddressingthesefactors.
Keywords
Composite index of anthropometric failure
under-5 children
nutritional status
Introduction :
Under-5 children constitute the most vulnerable segment of any community. Their nutritional status is a sensitive indicator of community health and nutrition. The pre-schoolers have to cope with the killer triad of diarrheal diseases, respiratory tract infection, and malnutrition, resulting in high morbidity and mortality.[1] One in every three malnourished children in the world lives in India.[2] Poor quality of infant and young child feeding practices are the major cause of malnutrition among the under-5 children of any society.[2] More than half of all child deaths are associated with malnutrition, which is accelerated by the weakened body's resistance to illness.[3]
In 2012, the World Health Assembly adopted the 2025 Global Targets for Maternal, Infant and Young Child Nutrition.[4] In 2015, Sustainable Development Goals had the objective of "ending all forms of malnutrition," challenging the world to think and act differently on malnutrition - to focus on all its faces and work to end it, for all people, by 2030.[4] Globally among under-5-children, 23.5% are stunted and 7% are wasted.[4] In India, 35.7% are underweight, 38.4% are stunted and 21% are wasted.[5] In West Bengal, 26.2% are under weight, 28.5% are stunted and 16.7% are wasted.[6]
While stunting (low height-for-age) is an indicator of chronic undernutrition due to prolonged food deprivation and/or illness, wasting (low weight-for-height) is an indicator of acute undernutrition, an end result of more recent food deprivation and /or illness.[7] The nutritional status of under- five children in the slums is very important because this is a vulnerable group which may fall prey to different types of communicable diseases that can spread easily due to high population density, poor hygiene, illiteracy and poor socioeconomic status in these areas.[2] There is another concern with the use of conventional indices. Weight-for-age is most commonly used to assess the nutritional status. This may be because underweight indicates both acute and chronic undernutrition. However, underweight is not the summation of children who are wasted and stunted. As a result, we might tend to miss out on children who are stunted and wasted if underweight is used as a sole indicator of nutritional status. An alternative indicator CIAF (Composite Index of anthropometric failure) was proposed by Svedberg in 2000[9] and further modified by Nandy et. al[10] Although CIAF is also a composite measure, it addresses the issue of overlap among various categories of under nutrition. The CIAF includes all children who are wasted, stunted or underweight, and their combinations (groups B-Y).
With this background in mind, this study was conducted to assess the nutritional status of under 5 children in a slum of Kolkata and to identify the factors affecting nutritional status of the study participants.
Materials And Methods :
The study was a community-based observational study with cross-sectional design. It was conducted over a period of three months (October to December 2017) in a slum of Kolkata under Urban Health Unit and Training Centre (UHU&TC), Chetla, which is the urban field practice area of All India Institute of Hygiene and Public Health (AIIH&PH), Kolkata.
Considering the prevalence of underweight in that urban area as 42%[11] with 95% level of significance and 20% relative error, and usingtheformula :
Sample size[11] = (Z1-α/2)2pq/L2
= 1.96X 1.96X42X 58/({20X42}/100)2 =133 (p = prevalence, q = 100-p, L = allowable error, Z1-α/2 for 95% confidence level = 1.96), the estimated minimum sample size was calculated to be 133. Line listing of all under-5 children in the study area was done and selection of study participants was done by simple random sampling. Those children whose mothers were not present at the time of data collection or did not give consent to participate were excluded. Four such children were excluded by exclusion criteria. The final sample size came to be 129.
After obtaining written informed consent from mothers ofthe under-5 children, face-to-face interview was conducted with a pre-designed and pre-tested schedule. This schedule was prepared according to the objectives of the study and was corrected by a group of experts of the institute. Pretesting was carried out among ten mothers of representative sample. After pretesting necessary modifications were made. Utmost care was taken to make the language as simple as possible so that the respondents, even if illiterate, could understand the questions easily.
All relevant information including socio demographic characteristics, relevant antenatal history, birth weight, feeding pattern, personal hygiene, morbidity within last 2 weeks, immunization, de-worming, use of Integrated Child Development Scheme (ICDS) services were gathered. Socioeconomic status was estimated according to the modified BG Prasad scale[12] (January 2017). Anthropometric measurements were recorded following standard operating procedures. The data included were weight, recumbent length (if the child is not able to stand without support), standing height and mid upper arm circumference (for children above 12 months). Portable analogue weighing machine and Salter weighing machine was used for weight measurement, non-stretchable measuring tape for measuring standing height and MUAC, Infantometer for measuring recumbent length and Maternal and Child Protection (MCP) Card (whenever available) especially for immunization were used.
The following operational definitions were used in the study.
A. World Health Organization-Z-Score System:
Wasting (acute malnutrition) was defined as a Weight for Height Z-score (WHZ) of < -2. Severe wasting is considered if WHZ is < -3.
Stunting (chronic malnutrition) was defined as a Height for Age Z-score (HAZ) of < -2. Severe stunting is considered if HAZ is < -3.
Underweight (mixed acute and chronic malnutrition)[9] was defined as Weight for Age Z-score (WAZ) of <-2. Severe underweight is considered if WAZ is < -3.
Mid upper arm circumference (MUAC): The cut-off point of 13.5 cm was used for identifying children with under nutrition.
B. Composite Index of Anthropometric Failure (CIAF):
Peter Svedberg[7] developed a model of six groups of children (A to F) to calculate CIAF. Nandy et al.[8] later modified the Svedberg's model by identifying an additional subgroup (Group Y: children who are only underweight). The CIAF excludes those children not in anthropometric failure (group A) and includes all children who are wasted, stunted, or underweight, and their combinations (groups B-Y).
I. Group A : No failure
II. Group B : Wasting only
III. Group C : Wasting and underweight
IV. Group D : Wasting, stunting, and underweight
V. Group E : Stunting and underweight
VI. Group F : Stunting only
VII. Group Y : Underweight only
All data collected were compiled and analysed using Statistical Package for Social Sciences (SPSS), version 16.0 (IBM Corp., Chicago). Descriptive and analytical results are presented through tables and association between variables was stated by bivariate and multivariable logistic regression. The study was approved by Institutional Ethics Committee.
Results:
The mean (±SD) age of under-5-chlldren was found to be 30.7 (±17.5) months ranging from 2 months to 58 months. Maximum children belonged to the age group of 47-58 months. Among them, 56.6% were male and 43.4% were female. AII children were Hindu by religion. 45% of mothers and majority of fathers (84.5%) of children had studied up to middle school. Among the mothers, 84.5% were home maker and 15.5% worked for pay. Father of majority of the children (67.4%) were unskilled labour.
According to modified BG Prasad Socio Economic Scale January 2017 majority of them belonged to lower middle class (56.6%), followed by middle class (39.5%), upper middle class (1.6%)and lower class (2.3%). All of them resided In pucca house. Drinking and domestic water source were i ntermitte nt ta p water su pply from munici paIity.
None of them had separate kitchen for cooking and they cooked either Inside the room or outside In the open space. The types of fuel usually used were wood (4.7%), kerosene (26.6%), Liquid Petroleum Gas (LPG) (5.4%) and mixed (63.3%) comprising of mainly LPG and kerosene. 64.3% of the families had the habit to throw excreta of younger children in the canal passing through the slum and rest used shared community latrine.
It was found that 43.3% of the mothers had early registration during pregnancy. All of them had four or more Antenatal Care (ANC) visits and their pregnancy were uneventful. All of them had institutional deliveries, 69% normal delivery and 31% caesarean section. Approximately 21% of the mothers reported to have delivered babies with low birth weight.
None of them had received pre-lacteal feed after birth.73 (59.3%) children had exclusive breast feeding up to 6 months of age. All of them started complementary feeding at the age of 6 months. 90.2% children continued breast feeding with complementary feeding beyond 2 years of age. They did not wash hands with soap and water before taking food and their mothers had adopted same practice before feeding. All children were immunized but MCP Card was available forll4 (88.4%) children at the time of data collection. Among the children,79 (61.2%) had long/dlrty and 50 (38.8%) clean/short nails, 24 (18.6%) were with clean and 105 (81.4%) with dirty clothes at the time of data collection. Mothers of about three-quarter of the children reported that their children walked outside barefooted.22.5% children availed ICDS services and 80% of them visited for 6 days a week. 96 (75%) had undergone dewormlng within last 6 months. 40.3% had illness within last 2 weeks, comprising of diarrhoea (3.9%), fever (10.9%), acute respiratory tract Infection (25.5%).
Out of total 129 children assessed, 31.8% were found to have anthropometric failure using CIAF. However, with standard anthropometric Indices such as weight-for-age, weight-for- helght, height-for-age, and mid upper arm circumference, 17.8% were underweight, 9.3% were wasted, 16.3% were stunted and 14% were undernourished respectively (Table 1).
| Characteristics | No. (%) |
|---|---|
| 1.Weight for Age | |
| Normal | 106(82.2) |
| Underweight (<-2 SD) | 23(17.8) |
| 2. Height for Age | |
| Normal | 108 (83.7) |
| Stunting (<-2SD) | 21 (16.3) |
| 3.Weight for Height | |
| Normal | 117(90.7) |
| Wasting (<-2 SD) | 12(9.3) |
| 4.Mid Upper Arm Circumference (n=105) | |
| Normal | 87(82.8) |
| Less than normal | 18 (17.2) |
| 5.Composite Index of Anthropometric Failure | |
| Group A (no failure) | 88(68.2) |
| Group B (wasting only) | 3(2.3) |
| Group C (wasting and underweight) | 9(7.0) |
| Group D (wasting, stunting, and underweight) | 0 |
| Group E (stuntingand underweight) | 6(4.7) |
| Group F (stunting only) | 15(11.6) |
| Group Y (underweight only) | 8(6.2) |
The enter method was used to perform logistic regression. In univariate low level of education, mothers with work for pay, low per capita income of family, low birth weight, high birth order, babies without exclusive breast feeding for first six months of age, increased morbidities, poor personal hygiene had higher odds for anthropometric failure and were statistically significant.
In multivariable binomial logistic regression, the statistically significant independent variables were considered. Literacy of mother [Adjusted odds ratio (AOR)-3.79 (1.39-10.33)], exclusive breast feeding [AOR-6.1 (1.80-8.79)], personal
hygienic practice [AOR-3.17 (1.02-10.02)] and morbidity profile [AOR-2.95 (1.13-7.72)] were found to be significantly associated with nutritional status (Table 2).
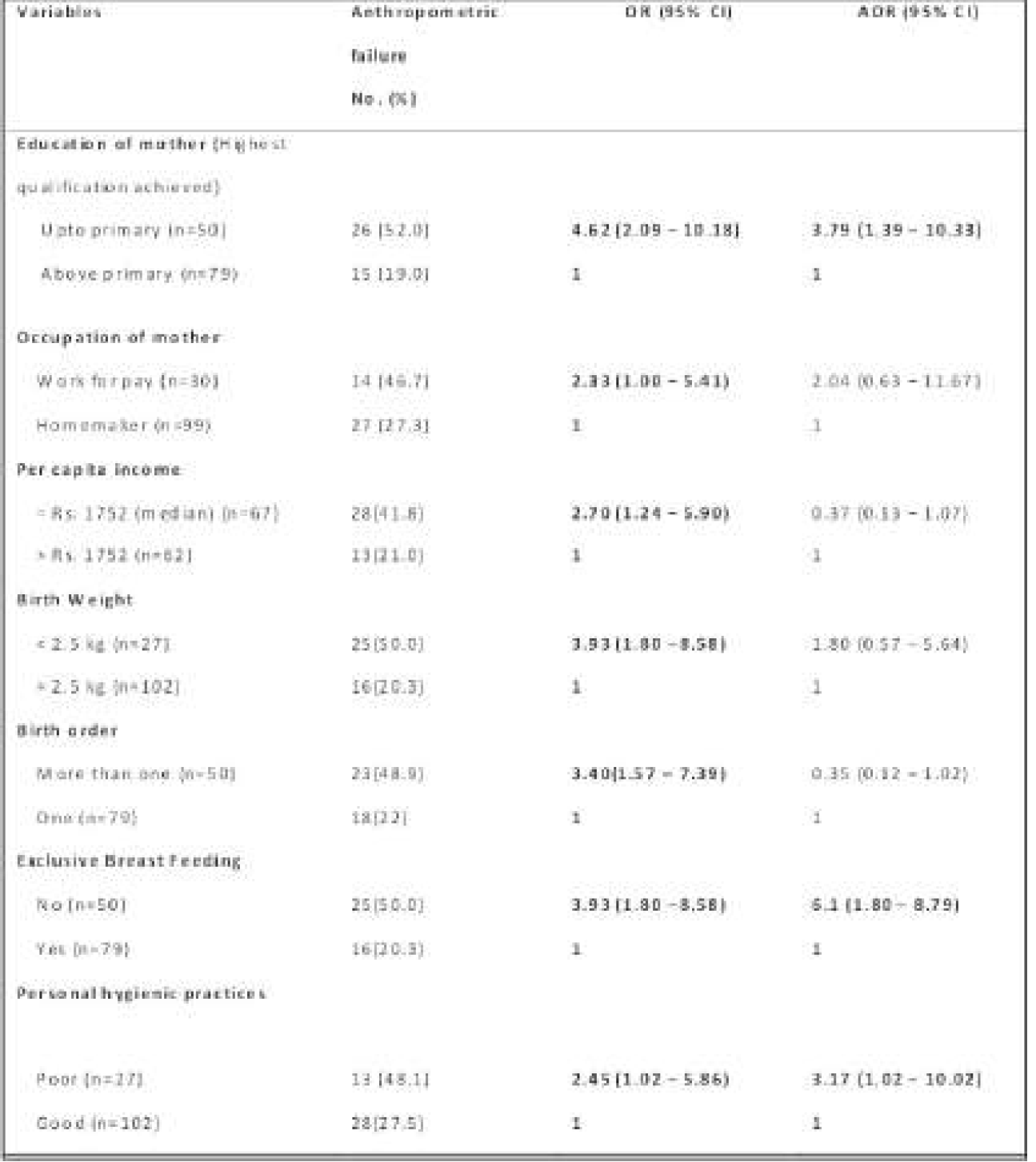
Nagelkarke R square was 0.42 which inferred that 42% variance in outcome (anthropometric failure) was explained by independent variables. Non-significant Hosmer- Lemeshow (0.40) test supported good statistical fit of the logistic regression model.
Discussion:
In the current study, 52% mothers with lower level of education had children with anthropometric failure which is similar to a study by Rastogi S et al.[13] where children of literate mothers were less likely be undernourished than children of illiterate mothers. This is also similar to another study by Shit S et al.[14] where children of literate mothers (68.5%) were less likely to have anthropometric failure than children of illiterate (92.3%) and just literate mothers (89.2%). In another study by Dasgupta A et al.[15] under nutrition was more among mothers with lower level of education (80.7%). A much higher proportion of anthropometric failure was found more among children with birth weight <2.5 kg (51.9%) than with birth weight ≥2.5kg (26.5%) and similar finding were reported in studies by Rastogi et al.[13]and Dasgupta A et al. in an urban slum[15] anda rural area of West Bengal. Under nutrition was also more among children of higher birth order in this study which is similar to the studies by Dasgupta A et al. [15,16]and Rastogi et al. [13]The study conducted by Mukhopadhyay et al.[17] found a higher prevalence of undernourished children in families with lower monthly income which was similar to the current study. In our study, faulty feeding practices and morbidities were common among children with anthropometric failure which was similar with the studies by Dewan D et al [18]and that by Solanki R et al.[19] In this study 31.8% of the children had anthropometric failure. Among them 17.3% were underweight, 9.3% wasted and 16.3% were stunted. This finding is lower than that noted in the study done in another study in urban West Bengal.[11]
Conclusion:
There are a large number of effective national programmes for the Indian children in regards to the common morbidities like Diarrhoea and ARI and common specific nutrient deficiencies like iron, Vitamin A and iodine. Beyond that there are programmes for improvement of general nutrition like the supplementary nutrition of ICDS and Mid-Day Meal Scheme. Inspite of all these efforts poor nutritional status of children continues to plague the Indian population as is apparent in this study. Therefore, improvement of all programmes related to the health of the under 5 must be given a priority with special emphasis on all the national nutrition programmes. The study identifies maternal education and care and infant and child feeding practices to have a bearing on the nutritional status of the children. Further large scale studies are warranted to determine the alleviation in the situation after addressing these factors.
Acknowledgement :
We acknowledge our colleagues of All India Institute of Hygiene and Public Health for their support. We also acknowledge the Officer-in-Charge of Chetla for allowing us to conduct the study. We are grateful to the study participants without whose support, we could have never been able to conduct the study.
Conflict of interest:
None
How to cite this article : Roychoudhury N, Pan T, Roy K, Paul B, Dasgupta A, Bandyopadhyay L. Assessment of Nutritional Status of Under-5 Children in A Slum of Kolkata, West Bengal: A Community Based Study. J Comprehensive Health 2019; 7(2): 23-28.
References :
- Why should 5000 children die in India every day? Major causesof death and managerial challenges. Vikalpa. 2010;35:9-19.
- [CrossRef] [Google Scholar]
- Complementary feeding. Available from: https://www.who.int/nutrition/topics/ complementary_feeding/en/ (accessed )
- [Google Scholar]
- Health Education to Villages. Available from: http://hetv.org/programmes/nutrition.htm. (accessed )
- [Google Scholar]
- Global Nutrition Report 2016: From Promise to Impact: Ending Malnutrition by 2030. Washington, DC; 2016.
- [CrossRef] [Google Scholar]
- Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee Technical Report Series 854. Geneva: WHO; 1995.
- [Google Scholar]
- Nutritional status of underfive children in urban slums of Pune. Int J Med Public Health. 2014;4:247-52.
- [CrossRef] [Google Scholar]
- Poverty and undernutrition: theory, measurement and policy. New Delhi: Oxford India Paperbacks; 2000.
- [CrossRef] [Google Scholar]
- Poverty, child undernutrition and morbidity: new evidence from India. Bulletin of the World Health Organization. 2005;83(3):210-216.
- [Google Scholar]
- Sample size determination in health studies: a practical manual. World Health Organization, Geneva 1991
- [Google Scholar]
- Socio-economic status scales updated for 2017. Int J Res Med Sci. 2017;5:3264-7.
- [CrossRef] [Google Scholar]
- Assessing Burden of Under-Nutrition among Underfive Children of Urban Slum by Using Composite Index of Anthropometric Failure in Ahmedabad City, Gujarat, India. National Journal of Community Medicine. 2017;8(8):496-500.
- [Google Scholar]
- Assessment of nutritional status by composite index for anthropometric failure: A study among slum children in Bankura, West Bengal. Indian J Public Health. 2012;56:305-7.
- [CrossRef] [PubMed] [Google Scholar]
- Composite index of anthropometric failure and its important correlates: a study among under- 5 children in a slum of Kolkata, West Bengal, India. International Journal of Medical Science and Public Health. 2015;4(3):414-419.
- [CrossRef] [Google Scholar]
- Assessment of Under Nutrition with Composite Index of Anthropometric Failure (CIAF) Among Under-Five Children in a Rural Area of West Bengal. Indian Journal of Community Health. 2014;26(2):132-138.
- [Google Scholar]
- Anthropometric Failure, a new approach to measure under nutrition: An experience from a rural community of West Bengal, India. J Indian Med Assoc. 2009;107:211-36.
- [Google Scholar]
- Predictors of anthropometric failure among under five slum children of Jammu, India. International Journal of Community Medicine and Public Health. 2016;3(1):367-372.
- [CrossRef] [Google Scholar]
- Measuring undernutrition through z-scores and Composite Index of Anthropometric Failure (CIAF): a study among slum children in Ahmedabad city, Gujarat. National Journal of Community Medicine. 2014;5(4):434-9.
- [Google Scholar]






