Translate this page into:
Addressing Malnutrition among Children – An Assessment of Dastak Abhiyan in Madhya Pradesh
Corresponding author: Dr. Vaibhav Patwardhan. Chhatri Bazar, Lashkar, Gwalior, M.P-474001. E-mail: vebhavpatwardhan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Patwardhan V, Kotwani P, Tiwari P, Saha S . Addressing Malnutrition among Children - An Assessment of Dastak Abhiyan in Madhya Pradesh. J Comprehensive Health. 2018; 6(1):37-41.
Abstract
Background:
The Dastak Abhiyan is considered a pioneer program of Government of Madhya Pradesh and was pilot tested in the month of November 2016. The program offers a basket of services (10 core activities) focused on the reduction of Under 5 mortality
Objectives:
In this study, we monitored the functioning and the implementation of 10 core activities of the Abhiyan in 4 districts of Madhya Pradesh viz. Jhabua, Sheopur, Raisen, and Bhopal.
Methods:
The study takes into account modified World Health Organization(WHO)'s 30x7 cluster sampling where 7 households were selected from 30 villages of 4 districts of Madhya Pradesh including 2 tribal and 1 high priority district.
Results:
We have observed that majority of the Front Line Health Workers (FLWs) were working as per the micro plan. We identified few gaps, such as FLWs missed on carrying out some of the activities viz. Blood Test, Mid Upper Arm Circumference measurement, demonstration of Oral Rehydration Solution preparation, and Handwashing.
Conclusion:
We found the need to strengthen inter-communication, to customize micro plan in consultation with the Auxiliary Nurse Midwife of that village. Our study also highlighted the need for supportive supervision, post-training assessment for FLWs to assess the knowledge gained by them during the training session.
Keywords
Dastak abhiyan
monitoring
Spot-Check
severe acute malnutrition
under 5 mortality
Introduction:
The infant mortality and under 5 mortality rate are the most critical indicators of a nation's progress in the health sector and thus, for the well-being of its children. India has significantly reduced its mortality indicators over a period of time. The Infant Mortality Rate (IMR) has declined from above 100 in the early 90s to the current rate of 38 per 1000 live births.[1] Talking about Madhya Pradesh the health indicators are slightly above the national average, with IMR 51 per 1000 live births and U-5mortality 65 per 1000 live births.[2] A greater proportion of these deaths in Under 5 children are attributed to malnutrition.[1]
Nutritional status and adequate growth of children can be assured by implementing infant and young child feeding practices ranging from exclusive breastfeeding to age- appropriate complementary feeding, especially diet diversity and its promotion at the community level.[3] Thus, declining the malnutrition in the state.
Yakoob et al. in their study suggests the inclusion of preventive zinc supplementation in public health programs to improve child health and survival.[4] Grewal T et al. in their study mentioned that variety of interrelated factors play a definitive role in determining health status if the group. Factors such as dietary practices, traditional beliefs, economic and educational level of the family, environmental sanitation and personal hygiene, maternal care, etc.[5] Studies also suggest that Vitamin A deficiency has been recognized as the leading cause of preventable pediatric blindness in developing countries.[6]
As per National Family Health Survey 4 (NFHS 4; 2015-2016 State Fact Sheet Madhya Pradesh), 68.9% of the children aged 6-59 months are anemic (<11 g/dl), 42% of the state's under-five children are stunted, 9.2% of the children in the state has Severe Acute Malnutrition (SAM). Only 34.5% children received the benefit of breastfeeding in the first hour of birth (early initiation of breastfeeding) and 58.2% children were exclusively breastfed in first 6 months of life.[2] Mishra C.P in his recent 2017 paper mentioned "In any country, primarily, three types of strategies (viz., legislative, service, and educational) can be adopted for freedom from malnutrition. If these approaches are executed optimally, they can serve as effective tools toward the fulfillment of the dream of malnutrition-free India."[7] Working on the same line, the GoMP came up with Dastak Abhiyan with focus on preventive and promotive aspects of the health of under-five children of the state. Claeson et al underline the importance of health programs and mentions "increasing the use of health services during pregnancy and delivery would lower child mortality".[8] The Dastak Abhiyan is based on active case finding by frontline health workers' involvement and with the support of Integrated Child Development Services (ICDS) workforce. The Abhiyan was pilot tested in 168 blocks of the state, which had poor full-immunization coverage in the year 2016 from16th– 30th November and showed positive reflections as per the GoMP officials.[9]
The program entails door-to-door visit of frontline health workers, thus the name Dastak, and was programmed for series of interventions listed below. The first phase of the campaign was launched throughout the state from 15th June to 15th July to cover every child aged 0 to5 years in the state. The campaign has to be carried out bi-annually in the months of June (Diarrhoea, SAM and malaria predominant season) and December (Pneumonia predominant season).
A Real-Time monitoring tool was developed to keep the track of children and was merged with SAMAGRA ID of the child and family. Samagra Unique Family ID is an 8-digit unique number assigned to a registered family by Government of Madhya Pradesh (GoMP) to provide benefits of all government schemes and services easily.)
The state took further initiatives to train the health workers specifically for Dastak Abhiyan. Three training sessions were carried out prior to Abhiyan.
The interventions included in the basket of services are: [10]
Active case finding of SAM and referral of medically complicated cases to Nutrition Rehabilitation Centres (NRCs).
Screening of childhood anemia and referral of severe anemic cases.
Vitamin A supplementation to all children from 9months to 59months.
Early identification and management of childhood Pneumonia in the community and need-based referral to the facility.
Raising community awareness on prevention of childhood Diarrhoea.
Extension of Infant and Young Child Feeding (IYCF) messages under Mother's Absolute Affection (MAA) program to the community doorstep.
Follow-up of Sick Newborn Care Unit (SNCU) and NRC discharged children.
Identification of children with visible congenital defects.
Testing of iodine adequacy in household salt in National Iodine Deficiency Disorder Control Program (NIDDCP) 14 Endemic districts.
Identification and basic treatment of all sick U5 children. These interventions are to be carried out by "Dastak team" also referred as "Dastak Dal" and encompass Auxiliary Nurse Midwife (ANM) or Multi Purpose Health Workers (MPW), Accredited Social Health Activist (ASHA), and Anganwadi Worker (AWW).
With this background the study was conducted to to assess whether the Dastak teams are carrying out the interventions correctly as per Dastak guidelines and to identify the gaps and challenges faced by Dastak team in the implementation of the 10 core activities of the Abhiyan.
METHODOLOGY:
Study Type: Observational study.
Study Design:
A structured questionnaire was used to collect data, and observations from the field were also taken into consideration to identify the gaps in the implementation of the program and its correlates.
Study Population:
The target population was the beneficiaries of the Dastak Abhiyan i.e. the households with U5 children of the state of Madhya Pradesh.
- Information about benefits of IFA syrup imparted
Sample and study setting:
Sample population for monitoring the activities carried out by FLWs were the 210 households with U5 children in 30 villages of 4 districts of Madhya Pradesh viz. Jhabua, Sheopur, Raisen, and Bhopal.
Sampling Technique:
Modified WHO's 30 cluster sampling technique was used as it was practically not possible to do purely simple random selection of villages.[11] However, random selection of villages was done based on their microplan in consultation with the block team in the above mentioned four districts and 7 households in each of the 30 villages interviewed with the help of a structured questionnaire. Purposive sampling was used to select 7 households within those 30 villages visited.
Method of Data Collection :
A structured questionnaire, which was used to monitor the activities, keeping the guidelines as the standard, had questions regarding timely receipt of required commodities by FLWs for the campaign. The tool also had questions on proper delivery of a basket of services (Blood Test, MUAC measurement, Iron Folic Acid (IFA) and Vitamin A supplementation, IYCF messages, Diarrhoea, Pneumonia, congenital anomalies) proposed as per the guidelines of the state government. It also helped to verify whether the positively identified children were referred to the respective referral unit or not. The quantitative data was analyzed to monitor the actual implementation of the program.
All the subjects who gave verbal consent were included in the study.
Results:
In our study, we found that 90% of the health workers were following the micro plan provided to them from the block. Also, the team was found complete at most of the places. But it was observed that no villager was aware of the Abhiyan when asked. The FLWs failed to create awareness in the community about the Abhiyan which was desired. Nearly 70% of villagers did not have a Ration card and thus not had Samagra ID as well.
- Information about benefits of Vit. A imparted
The concept of Dastak kit bag was introduced to help the ANM carry all the necessary drugs and commodities required for performing 10-core activities under the Abhiyan. It had separate compartments for separate items, so as to carry out the task without any chaos. Almost 50% of the ANM did not have Dastak kit bag. Though kit bag was not a major issue as all the necessary drugs and commodities were present with the ANM for uninterrupted functioning of the program.
Dastak cue cards, that had a pictorial representation of the program activities to increase the effectiveness of the behavioral change messages, failed to reach the entire districts of Jhabua and Sheopur even after the inception of the program.
During the Dastak spot-check, it was found that 1 ANM was on leave and no Dastak activities were found in that village. Also, there was no backup team deployed in the region to carry out the program activities as per the micro-plan.
In our study, we found that FLWs performs the blood test at 89.5% of the households. While MUAC was measured in 90.19% of the total households visited. During the visit made by the FLWs for the campaign, 95.5% of the children were found healthy, 3.5% of the children were advised home- based care, 0.5% of the children were advised to visit NRC as the child was identified as severely malnourished and the remaining 0.5% was advised hospitalization as the child was positively identified for anaemia. The advice was given after performing the activities at the doorsteps of the beneficiaries.
Of all the children observed and checked in the sample population, only a single case of malnutrition and anemia was observed during the visits and was referred to NRC and Community Health Centres (CHCs)/district hospital (as per the availability of blood transfusion facility) respectively, for the same.
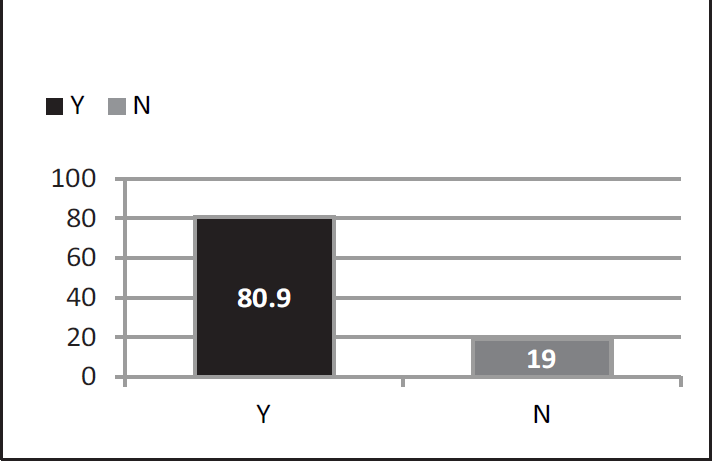
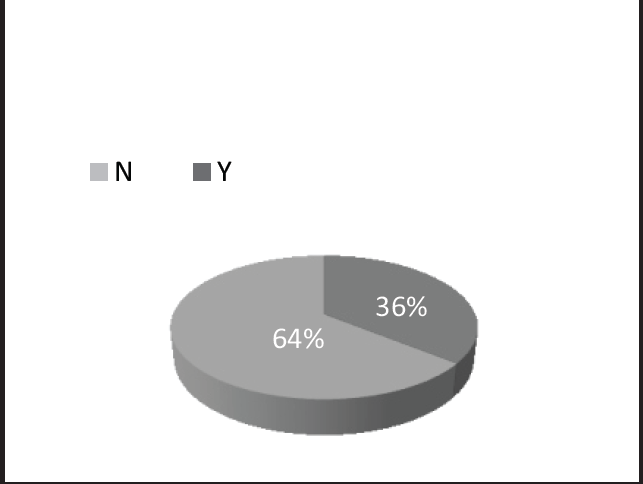
Under National Iron Plus Initiative (NIPI), it is mandatory to give proper dose of Iron-folic acid syrup biweekly to the child. Dastak Abhiyan entails the delivery of information about the benefits of IFA to the community. Information regarding benefits and dosage of IFA and Vitamin A supplementation was to be imparted by FLWs as a part of the campaign. Though the information was imparted to only 64% of households, 90% of the houses visited received correct dose of Vitamin A supplementation.
Only 7 cases (<4% of children screened during the Spot check) were <9 months old and hence were not eligible for Vitamin A. Thus, these cases were exempted from the calculation of activities for Vitamin A supplementation. Households, where Vitamin A supplementation was not given to the child, received the supplement in the past 4-6 month.
In 6.63% of all the houses visited, the team did not perform any activities at the doorstep but called the mother with her child to the Anganwadi center. While in 2.84%of the houses ANM went to school for mass administration of Vitamin A supplementation to the children.
Hence these households were not considered in calculations for IFA and Vitamin A supplementation.
No children with congenital defect were found among all the children screened. 1 case of developmental deformity in bones was observed and the child was referred to district hospital by the Dastak team but the family was reluctant to follow the advice.
Optimal IYCF practices can bring down the IMR/ child mortality rates by almost 20%. ANM with her Dastak team informed the 63% of the households about the benefits of breastfeeding and its early initiation within the first hour of birth to the pregnant mother, while the remaining 37% of them were not informed to do so.
More than half of the houses were informed about exclusive breastfeeding to the lactating mother in households where the child was less than 6 months of age. But none of them discussed the details of breastfeeding. No team talked about the time duration to feed the baby with each breast. Less than 5% talked about how many times a child should be fed in a day Dastak teams informed the mother about the continuation of breastfeeding to the child for at least 2 years and about complementary breastfeeding after 6 months of age of the child. They were also informed about the continuation of breastfeeding even during diarrhea or any other illness.
Of all the cases observed, no child with danger signs like cyanosis, tachypnoea, hypothermic or any critically ill child was found. During our study, no child was positively identified with pneumonia.
O.R.S packets had to be distributed to all the households where Dastak Abhiyan activities were carried out. 97% households received the ORS packets, but, when it came to the demonstration of ORS preparation and demonstration of hand-washing, the percentage dropped to 83%. And 52% of the houses received information regarding the benefits of the ORS and 11% of houses received information about an age-wise dose of ORS. One child, of all the cases, was positively identified for diarrhea and was given ORS packets and Zinc tablets for 14 days by the team. Salt testing was another component of the activities under Dastak but was not applicable to any of the districts chosen for study.
Discussion and Recommendations:
The study revolves around the activities performed by FLWs and their adherence to the prescribed guidelines. The ANMs were following the protocols during the implementation of Dastak activities in a reasonably large proportion.
The first major gap identified was the lack of awareness within the community about the Abhiyan. None of the households visited knew about the campaign and its activities. The FLWs reasoned that they were engaged with another program until a day before the start of Dastak Abhiyan hence could not spare time for the awareness generation of this new program. The planning of the programs should be done such that the FLWs find enough time for the preparatory activities of the upcoming campaign.
The Dastak Kitbag was sponsored by United Nations International Children's Emergency Fund (UNICEF) and was supposed to be distributed before the inception of the program. However, there was a delay in receiving the product by the state in sufficient amount, which led to failure in receipt of the kit bags by the FLWs of two of the four districts visited. The sponsors must be notified prior and procurement and distribution of all the necessary commodities have to be done before the inception of the Campaign.
The same scenario, as that of Dastak Kit bags, was observed regarding the receipt of Dastak Cue Cards which need to be procured and distributed before the start of the campaign. In the districts, which received Dastak Cue Cards, the FLWs did not use it during their visit which signifies the wastage of resources. This can be taken care in the future by emphasizing the utility of Cue Cards in the training session for the purpose of behavior change in the community.
With a prevalence of 68.9% anemia and 9.2% severe malnutrition in U5 population in the state, finding only a single case of anemia and malnutrition in the sample observed does not resemble with the actual burden of the disease in the state. This may be suggestive of poor quality of work performed by FLWs. The FLWs must be sensitized regarding actual status of the disease in the state so that they understand the importance of each and every activity planned in the campaign.
As our finding suggests, in 10% of the households the FLWs failed to measure MUAC in spite of the training given to them for the same. 19% of the households did not receive information about the benefits of IFA syrup, while 36% did not receive information about benefits of Vitamin A supplementation. In 37% of the households, messages of infant and young child feeding practices were not delivered. About ORS related activities, 17% of the households did not receive a demonstration of ORS, 48% were not informed about benefits of ORS and 89% were not explained about the age-wise dosage of ORS. The above figures show that the FLWs missed performing few of the activities, which calls for the need of supportive supervision.
Though the program planning was excellent, there were few breaches that need to be addressed in upcoming phases of the campaign for further expanding the success ratio. The time duration allotted to travel from house to house in each village cannot be standardized and has to be addressed as per the need. The hamlets of Dungra village of Jhabua district had houses distantly situated on hillocks and hence took more time and efforts to cover the same. This could be one of the reason because of which the FLWs called villagers at Anganwadi Centre, School, etc. for carrying out the activities of the campaign.
The Samagra IDs or even ration cards were not available in many of the households which made the reporting difficult. Similarly, the reporting format provided to the teams had errors like missing parents' or child's names and had names of children above the age limit for the campaign. This needs rectification and up-gradation of the database. However, the ANMs were given authority to make changes in the list provided to them as per the need.
The WHO color scale provided for hemoglobin estimation was not appropriate. As per majority of the ANMs, the color shades could not be appreciated distinctly and hence matching of the blood sample with color shades for hemoglobin estimation was difficult. Corrective actions were taken by the state authority so that such mistakes may not occur in future.
Despite all the issues and gaps in the system, most of the FLWs were working hard on the field for successful execution of the program.
The Abhiyan seemed to be working fairly well in the field which can be deduced by the amount of satisfaction on the face of the beneficiary when the services were rendered to their child by the FLWs.
Conflicts of Interest:
Nil
References:
- Reducing stunting in India: what investments are needed? Maternal & child nutrition. 2016;12(S1):249-52.
- [CrossRef] [PubMed] [Google Scholar]
- State Factsheet Madhya Pradesh. http://rchiips.org/NFHS/ pdf/NFHS4/MP FactSheet.pdf (retrieved on 20/07/2017)
- [Google Scholar]
- Infant and young child feeding practices and child undernutrition in Bangladesh: insights from nationally representative data. Public health nutrition (9):1697-704.
- [CrossRef] [PubMed] [Google Scholar]
- Preventive zinc supplementation in developing countries: impact on mortality and morbidity due to diarrhea, pneumonia and malaria. BMC Public health. 2011;11(3):S23.
- [CrossRef] [PubMed] [Google Scholar]
- Etiology of malnutrition in rural Indian preschool children (Madhya Pradesh) Journal of Tropical Pediatrics. 1973;19(3):265-70.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin A Deficiency: Health, Survival and Vision. The American Journal of Clinical Nutrition. 1997;65(1):173-4.
- [Google Scholar]
- Malnutrition-free India: Dream or reality. Indian Journal of Public Health. 2017;61(3):155.
- [CrossRef] [PubMed] [Google Scholar]
- Reducing child mortality in India in the new millennium. Bulletin of the World Health Organization. 2000;78(10):1192-9.
- [Google Scholar]
- (unpublished concept note developed by Department of Child Health Nutrition, National Health Mission Madhya Pradesh. reviewed on 20/07/2017)
- [Google Scholar]
- (unpublished state guidelines developed by Department of Child Health Nutrition, National Health Mission Madhya Pradesh. reviewed on 20/07/2017)
- [Google Scholar]
- A simplified general method for cluster-sample surveys of health in developing countries.
- [Google Scholar]






