Translate this page into:
Residence Inequality of Maternal Health Service Utilization among Women in Somaliland: An Analysis from the Somaliland Demographic Health Survey in 2020
*Corresponding author: Abdilaahi Yusuf Nuh, Department of Epidemiology, Jimma University, Jimma, Ethiopia. abdilaahi.yus@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nuh AY. Residence Inequality of Maternal Health Service Utilization among Women in Somaliland: An Analysis from the Somaliland Demographic Health Survey in 2020. J Compr Health. 2025;13:89-95. doi: 10.25259/JCH_59_2024
Abstract
This study examines the factors influencing maternal health service utilization in Somaliland, where there is significant disparity in access based on place of residence. Previous studies indicate that women from higher-income households are more likely to use maternal health services. Using data from the 2020 Somaliland Demographic Health Survey (SLDHS), which included a weighted sample of 2,991 women of reproductive age from all six regions of Somaliland, the study investigates maternal health service utilization patterns. The results show that the majority of participants were aged 25-29 years, with a high percentage being married (94%) and having primary education (80.9%). A substantial portion of women lived in nomadic (38.1%) or rural (34.4%) areas, with 37.6% from the lowest wealth category. Among the women surveyed, 28.9% received antenatal care (ANC), 4.5% received postnatal care (PNC), and 76.8% delivered at home. Urban women had the highest utilization rates for ANC (48.15%), delivery (55.7%), and PNC (57.46%), while nomadic women had the lowest rates (ANC 13.39%, delivery 9.02%, PNC 11.94%). These results highlight significant geographical disparities in access to maternal health services, with urban women benefiting from considerably higher utilization rates. To address these inequities, it is recommended that policymakers implement targeted health programs for rural and nomadic populations, such as mobile health clinics and improved healthcare infrastructure.
Keywords
Antenatal services
Delivery services
Maternal health services
Postnatal services
INTRODUCTION
Maternal health refers to women’s health during pregnancy, delivery, and the post-delivery period for the maximum well-being of both the mothers and the infants.1,2 Studies have established that appropriate utilization of maternal health services, such as antenatal care (ANC), skilled delivery service, and postnatal care (PNC), is essential in improving maternal health outcomes. Service coverage has been identified as a way to reduce maternal mortality rates in developing countries.3,4 The use of appropriate levels of maternal health services is crucial for creating safe motherhood and has significant impacts on the mothers’ outcomes as well as those of their offspring.5
Maternal health remains one of the most important matters related to health globally and is of high interest to governments and policymakers, particularly in resource-limited regions.6 It forms a cornerstone in the 2015 United Nations’ Sustainable Development Goals target 3.1, with efforts toward its reduction to <70 maternal deaths per 100000 live births by 2030.7,8 However, Maternal mortality rate (MMR) remains one of the major killers among females in Africa. The Sub-Saharan Africa (SSA) region, where most West African countries are located, has the highest rates of maternal deaths and contributes 70%, or 202,000 deaths, to maternal mortality worldwide.9
ANC is critically important for reductions in mortality through early identification and management of complications, optimization of nutrition, and prenatal education, including promoting healthy behaviors.10 Skilled delivery services are essential in ensuring safe delivery, managing complications that might arise from delivery, and quick responses in emergencies.11 It is also necessary to have PNC following childbirth so that complications such as postpartum hemorrhage and maternal and infant infections (sepsis) can be identified and treated.12 For this reason, there has been international advocacy to ensure adequate provision of services as a continuum for improving maternal and child health by reducing morbidities and mortality.12
The use of maternal health services was not evenly distributed worldwide by regions. Studies conducted in Bangladesh, Pakistan, and India indicated inequalities in maternal healthcare service utilization regarding skilled birth attendance, ANC visits, and PNC. These were linked with socioeconomic factors such as the wealth status, educational status of husbands and mothers, and place of residence.13-15 Studies in most African countries also reported disparities in the use of maternal healthcare services.16-20 Still, a multicountry study conducted in 36 SSA countries identified inequalities in ANC services due to socioeconomic factors.21,22 The same study found that four or more ANC visits are concentrated among the wealthiest segments of the population in nine African countries.23 Other studies focused on SSA, including Kenya and Zimbabwe, found that skilled birth attendance and ANC services were more accessible to people of high socioeconomic status.24
Data from the Somaliland Health and Demographic Survey of 2020 show that even though 47% of women received ANC from a skilled provider in their last pregnancy, many births still occur outside health facilities without skilled birth attendance.25 It also finds that there are large sociodemographic differentials in the use of maternal health services, where women from rural, nomadic groups and those from economically poor backgrounds face significant obstacles in accessing maternal healthcare services. These result from a distance to health facilities, financial problems, and cultural behaviors that may hinder the utilization of formal healthcare services.25
Thus, this study aims to analyze the determinants of maternal health service utilization among women in Somaliland using data from SLHDS 2020. This will give way to findings on barriers and facilitators regarding access to maternal health, informing strategies for improving service coverage to reduce maternal health disparities within the country.
Objectives of the study
To assess the sociodemographic factors affecting the utilization of maternal health services
To evaluate the impact of geographic location on access to antenatal, delivery, and PNC.
MATERIAL AND METHODS
Design, data source, and source of population
This study is a secondary analysis based on data from the Somaliland Demographic and Health Survey 2020 (SLDHS 2020). The SLDHS 2020 is the first-ever comprehensive household survey of demographic and health data from all six central regions of Somaliland. The participants targeted by this survey were women aged 15–49 years. The survey is a multistage probability sample, wherein each region was further divided into urban, rural, and nomadic residential areas, adding up to 18 equal strata. Within each stratum, 35 primary sample size units (PSUs) were randomly selected from urban and rural areas, and 10 PSUs were chosen in nomadic areas. Only 10 secondary sample size units (SSUs) were randomly selected from 35 listed PSUs in the urban and rural strata. Finally, from each selected PSU, 30 households were randomly selected, and all the eligible women aged 15– 49 years within those households were invited to participate in the survey. The data on maternal and children under 5 years of age health status were collected from all women through interviews. Face-to-face interviews were conducted using pre-tested questionnaires by trained interviewers.
The SLDHS interviewed 7137 women aged 15–49 from a nationally representative sample of 8212 households. A response rate of 76.5% was achieved by 5460. For the number of women interviewed, data were collected on ANC services from 2991 individuals, delivery services for 5826, and PNC services for 2991.
Data management and analysis
Data analysis was performed using the statistical software STATA for Windows Version 17.0. The results were determined based on the standard error, P-value, and a 95% confidence interval.
Measurements of variables of the study
Outcome variable
The outcome variable in this study was the level of utilization of maternal health services derived from the different care: ANC, skilled delivery services (SDS), and PNC. ANC uptake was coded as a binary outcome, where 0 represents women who did not get the service and 1 represents those who had at least a visit during their most recent pregnancy. The place of delivery was used as an indicator of SDS: 0 was for those who delivered outside the medical facility and 1 for those who delivered in it or received assistance from a skilled healthcare provider during delivery on the part of a doctor, nurse, midwife, public health, or certified community health worker. PNC receipt was then dichotomized as 1 for women receiving the postpartum checkup within the first 2 months after birth and 0 for those who did not. A composite index was created by combining all three variables to produce a single outcome variable called maternal health service utilization, which has a minimum and a maximum value of 0 and 3, respectively. This was further categorized into three: Not utilized for those who used none of the three services, partially utilized for those who used one or two of the services, and adequately utilized for those who used all the services. Previous studies utilized similar classification methods in determining the “no,” “partial,” and “adequate” service uptake.26
Explanatory variables
The potential factors of maternal health service utilization have been extracted from the dataset after reviewing related and recent literature. Because the demographic health survey (DHS) data are hierarchical, the variables were categorized as individual and community-level factors. Individual-level factors were features unique to each woman and were classified as sociodemographic, obstetric, and healthcare-related characteristics. Community-level factors, such as place of residence and community poverty, were also considered.
Method of analysis
I used multilevel modeling considering the nested nature of the DHS data, in which women were nested within households and households within clusters. This helps avoid biased estimates for parameters that arise with single-level analysis.27 Since the outcome variable had three response categories: Somewhat utilized, somewhat utilized, and completely utilized, this study used multilevel mixed-effect multinomial logistic regression. This approach addresses the variables’ nested nature, allowing for a more valid analysis of their associations at different levels of the hierarchy.
RESULTS
Sociodemographic, socioeconomic, and obstetric characteristics of women (15–49)
The household age group 25–29 was the most represented, with 28.1%, followed by the age groups 30–34 and 35–39, at 23.3% and 19%, respectively, while the age groups 15–19 and 45–49 had the least representation. Most women, 94%, were married; 80.9% had primary education as the highest level attended. A large number resided in a nomadic setting, 38.1%, or rural area, 34.4%, while the largest proportion originated from the Sool region, 24.2%. The lowest wealth status category had the highest proportion at 37.6%, while 43.6% had six or more children. Only 28.9% of participants received ANC services, further declining to 4.5% regarding PNC service utilization. Deliveries occurred mostly at home with a percentage of 76.8%, while 74.2% of the participants owned mobile phones and 25.8% of the participants did not [Table 1].
| Variables | Categories | Frequency | Percentage | Cumulative |
|---|---|---|---|---|
| Age in 5-year groups | 15–19 | 229 | 3.21 | 3.21 |
| 20–24 | 1168 | 16.38 | 19.59 | |
| 25–29 | 2005 | 28.11 | 47.7 | |
| 30–34 | 1659 | 23.26 | 70.96 | |
| 35–39 | 1357 | 19.03 | 89.99 | |
| 40–44 | 519 | 7.28 | 97.27 | |
| 45–49 | 195 | 2.73 | 100 | |
| Current marital status | Married | 6709 | 94 | 94 |
| Married | 266 | 3.73 | 97.73 | |
| Married | 162 | 2.27 | 100 | |
| Highest educational level | Primary | 973 | 80.88 | 80.88 |
| Secondary | 158 | 13.13 | 94.01 | |
| Higher | 72 | 5.99 | 100 | |
| Region | Awdal | 887 | 12.43 | 12.43 |
| Woqooyi Galbeed | 1515 | 21.23 | 33.66 | |
| Togdheer | 1644 | 23.03 | 56.69 | |
| Sool | 1729 | 24.23 | 80.92 | |
| Sanaag | 1362 | 19.08 | 100 | |
| Type of place of residence | Rural | 2455 | 34.4 | 34.4 |
| Urban | 1962 | 27.49 | 61.89 | |
| Nomadic | 2720 | 38.11 | 100 | |
| Wealth index combined | Lowest | 2680 | 37.55 | 37.55 |
| Second | 1231 | 17.25 | 54.8 | |
| Middle | 756 | 10.59 | 65.39 | |
| Fourth | 1097 | 15.37 | 80.76 | |
| Highest | 1373 | 19.24 | 100 | |
| Number of children | None | 378 | 17.79 | 17.79 |
| 1–2 | 42 | 1.98 | 19.76 | |
| 3–4 | 169 | 7.95 | 27.72 | |
| 5–6 | 609 | 28.66 | 56.38 | |
| 6+ | 927 | 43.62 | 100.00 | |
| Antenatal care services | Yes | 866 | 28.95 | 28.95 |
| No | 2090 | 69.88 | 98.83 | |
| Missing | 35 | 1.17 | 100.00 | |
| Place of delivery | Home | 4474 | 76.79 | 76.79 |
| Health institution | 1352 | 23.21 | 100.00 | |
| Post-antenatal care services | Yes | 134 | 4.48 | 4.48 |
| No | 2812 | 94.02 | 98.50 | |
| Missing | 45 | 1.50 | 100.00 | |
| Owns a mobile telephone | Yes | 5294 | 74.18 | 74.18 |
| No | 1843 | 25.82 | 100 |
SLDHS: Somaliland demographic and health survey
Maternal health service utilization (ANC, delivery service, and PNC) by place of residence
ANC services utilization is highest among urban women, which are 48.15%, followed by rural women, which are 38.45%, while the lowest among nomadic women, at 13.39%. A majority of those with no access to ANC is among nomadic women, at 48.09%, followed by rural women, at 31.77%, while among urban women, it constitutes only 20.14%. Delivery service data also depict that urban residents are the most likely to use health institution deliveries, standing at 55.7%, though the proportion for rural women stands at 35.28%, while for nomadic women, it is as low as 9.02%. During post-ANC, urban residents again emerge as those most likely to receive such care, at 57.46%, while nomadic women have limited access at 11.94%. These figures reveal that there is a trend where urban women always top the list in the utilization of maternal health services, while nomadic women are always the least in health service utilization across all categories [Table 2].
| Variables | Categories | Type of place of residence | |||
|---|---|---|---|---|---|
| Rural no. (%) | Urban no. (%) | Nomadic no. (%) | Total no. (%) | ||
| Antenatal care services | Yes | 333 (38.45) | 417 (48.15) | 116 (13.39) | 866 (100) |
| No | 664 (31.77) | 421 (20.14) | 1005 (48.09) | 2090 (100) | |
| Missing | 9 (25.71) | 4 (11.43) | 22 (62.86) | 35 (100) | |
| Total | 1006 (33.63) | 842 (28.15) | 1143 (38.21) | 2991 (100) | |
| Delivery service | No | 477 (35.28) | 753 (55.70) | 122 (9.02) | 1352 (100) |
| Yes | 1446 (32.32) | 720 (16.09) | 2308 (51.59) | 4474 (100) | |
| Total | 1923 (33.01) | 1473 (25.28) | 2430 (41.71) | 5826 (100) | |
| Post-antenatal care services | Yes | 41 (30.60) | 77 (57.46) | 16 (11.94) | 134 (100) |
| No | 959 (34.10) | 751 (26.71) | 1102 (39.19) | 2812 (100) | |
| Missing | 6 (13.33) | 14 (31.11) | 25 (55.56) | 45 (100) | |
| Total | 1006 (33.63) | 842 (28.15) | 1143 (38.21) | 2991 (100) | |
ANC: Antenatal care, PNC: Postnatal care
Place of residence inequality of maternal health service utilization
All three maternal health services – ANC, delivery, and PNC – show geographical inequalities that are statistically significant, as the P-values for all stand at 0.000. The concentration index (CI) for ANC services is positive, which suggests that ANC utilization is more concentrated among urban residence women. Delivery services show the greatest inequality in access, with the highest CI, while urban residence women are significantly more likely to utilize delivery services. PNC services have the lowest CI, yet they still record a positive value, meaning urban residence women are more likely than their nomadic counterparts to access PNC services [Table 3]. The concentration curve indicates an evident difference in the use of maternal health services by geographical location [Figures 1-3].
| Maternal Health services | No. of observation | Standard error | (95% confidence interval) | P-value |
|---|---|---|---|---|
| ANC Service | 5826 | 0.0051 | 0.0434–0.0633 | 0.000 |
| Delivery Service | 2991 | 0.004 | 0.0866–0.1021 | 0.000 |
| PNC Service | 2991 | 0.0042 | 0.0099–0.0264 | 0.000 |
ANC: Antenatal care, PNC: Postnatal care
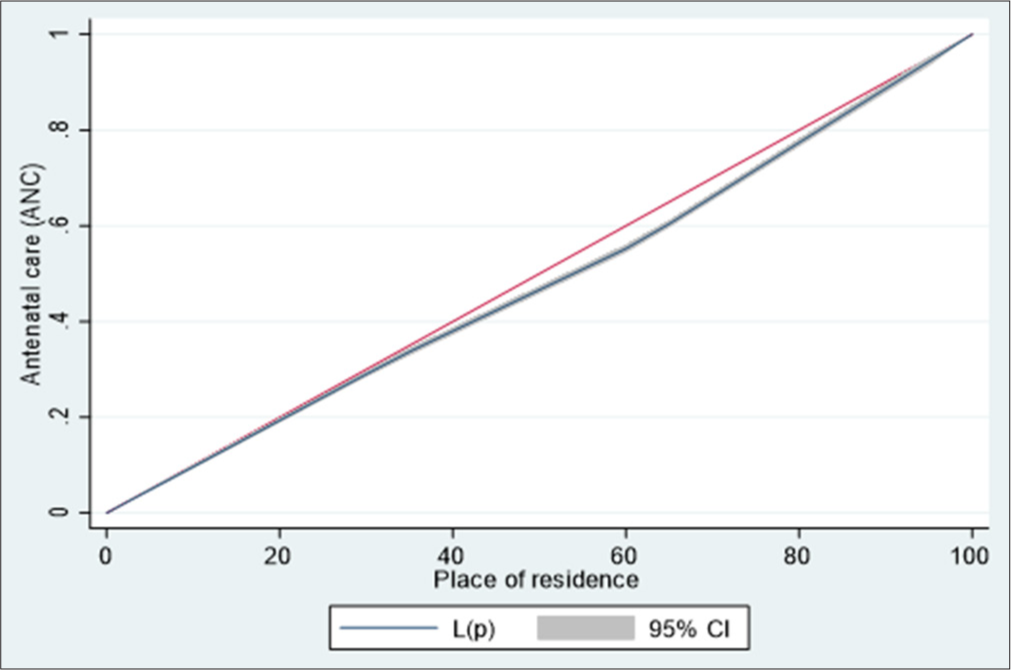
- Lorenz curve of antenatal care service utilization by household place of residence among women in the age group (15– 49). CI: Confidence interval.
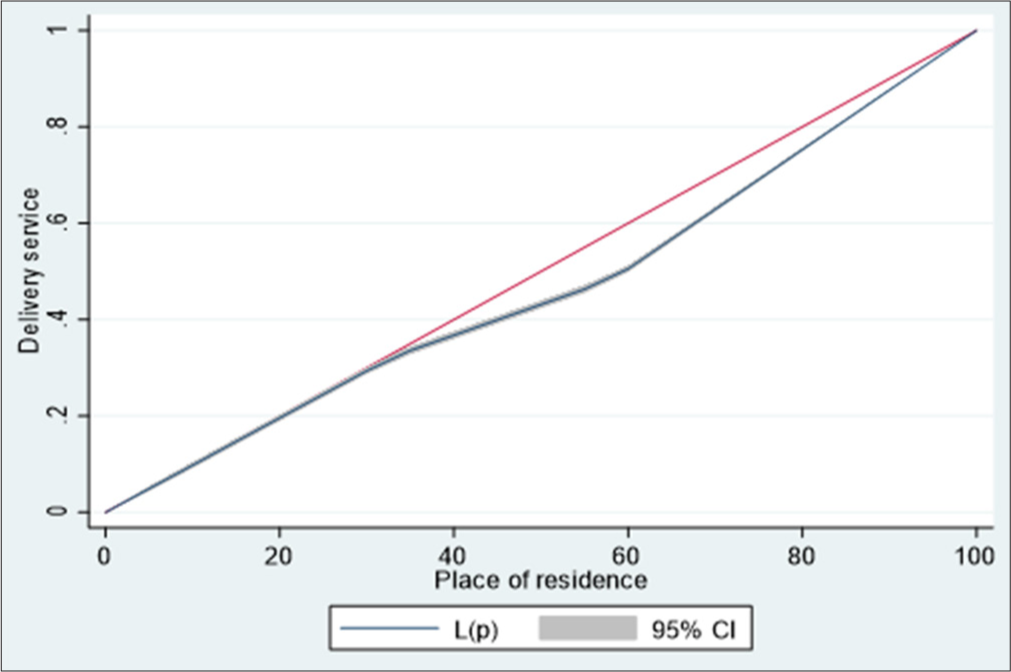
- Lorenz curve of delivery service utilization by household place of residence among women in the age group (15–49). CI: Confidence interval.
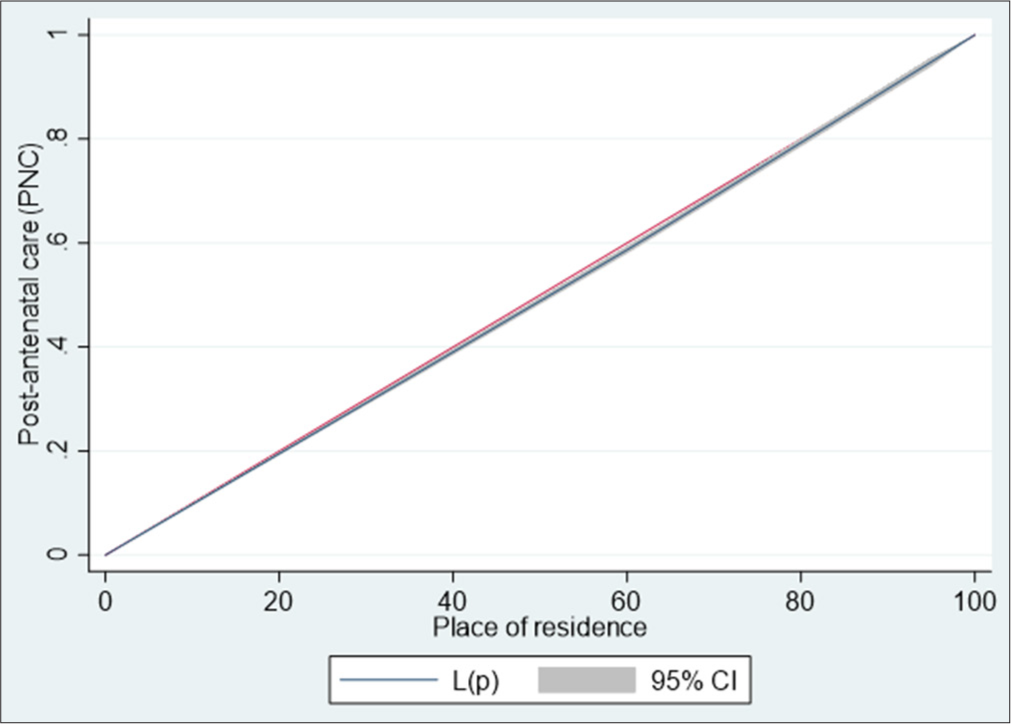
- Lorenz Curve of Post-natal care service utilization by household place of residence among women in the age group (15–49). CI: Confidence interval.
DISCUSSION
The study findings indicate that the level of utilization of maternal health services, ANC, delivery services, and PNC differs significantly by different places of residence in our population. Urban women had the highest proportions in all maternal health services: ANC service utilization stood at 48.15%, the utilization of delivery services at 55.7%, and PNC access stood at 57.46%. In contrast, the non-sedentary women have abysmally poor service utilization −13.39% received ANC services, 9.02% delivered services, and as low as 11.94% received PNC services. These results indicate that urban women have better access to maternal health services than their rural and nomadic counterparts. The large proportion of nomadic women not using ANC services and delivery services is 48.09% and 90.98%, respectively, showing a critical gap in health provision for this vulnerable group.
Place of residence inequality of Maternal Health service utilization. Rural women face critical barriers in accessing health facilities; consequently, home birth delivery by unskilled attendants becomes a regular scenario. For instance, studies in Ethiopia have shown that rural residence is a critical determinant of maternal health service utilization, with rural women less likely to receive skilled birth attendance compared to their urban counterparts.28
This trend is echoed in Somaliland, where the limited availability of healthcare facilities in rural areas exacerbates the challenges faced by women seeking maternal health services.29 The lack of transportation and poor infrastructure further compound these issues, making it difficult for women to access necessary care during pregnancy and childbirth.29,30
Another very vital and significant cause of the inequality in maternal health service utilization is socioeconomic status. According to available studies, relatively richer women tend to get ANC, skilled birth attendance (SBA), and PNC as opposed to relatively poorer women.31,32 This disparity, based on wealth, is consistent across the various African contexts and thus infers that economic barriers to access to maternal health services are very significant.31 In Somaliland, the economic challenges faced by many families, coupled with the historical context of civil unrest, have led to a healthcare system unable to meet the needs of its population.29
Educational attainment also emerges as a critical determinant in the utilization of maternal health services. Women with higher levels of education tend to know more about healthcare services and thus are more likely to seek care during pregnancy and childbirth.33,34 This relationship between education and health service utilization is well documented, with studies indicating that maternal education significantly influences the likelihood of receiving skilled care during delivery.34 In Somaliland, where educational opportunities may be limited, particularly for women, this can lead to lower rates of service utilization and poorer maternal health outcomes.29
Besides, the interplay among residence, socioeconomic status, and education presents a very complex landscape of inequality in maternal health service utilization. For instance, rural dwellings, low socioeconomic status, and a low level of education combine to impose multiple barriers that drastically decrease the probability of women receiving necessary maternal health services.31,32
CONCLUSION
This study has shown great disparities by place of residence in the utilization of maternal health services, with urban women receiving notably higher access to ANC, delivery services, and PNC compared with rural and nomadic women. These findings underscore the need for targeted policy action as an urgent intervention to bridge these gaps and assure equity in access to maternal health services for all women, especially those from sections that have hitherto been under-served. Policymakers must, therefore, focus on designing and implementing specific health programs for nomadic populations, including mobile health clinics, healthcare infrastructure, and resource distribution in rural and nomadic areas.
Ethical approval
The research/study was approved by the Institutional Review Board at Somaliland Central of Statistics Ref No. SLCS/212/2024, dated 1st September 2024.
Declaration of patient consent
The authors confirm that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- WHO Recommendations in Maternal Health. 2022. Available from: https://www.who.int/publications/i/item/WHO-MCA-17.10 [Last accessed on 2024 Nov 02]
- [Google Scholar]
- Global Inequality in Maternal Health Care Service Utilization: Implications for Sustainable Development Goals. Health Equity. 2019;3:145-54.
- [CrossRef] [PubMed] [Google Scholar]
- Improving Access and Utilization of Maternal Healthcare Services through Focused Antenatal Care in Rural Ghana: A Qualitative Study. Adv Public Health. 2019;2019:9181758.
- [CrossRef] [Google Scholar]
- Prevalence and Determinants of Maternal Healthcare Utilisation among Young Women in Sub-Saharan Africa: Cross-sectional Analyses of Demographic and Health Survey Data. BMC Public Health. 2022;22:647.
- [CrossRef] [PubMed] [Google Scholar]
- Spatial Clustering of Maternal Health Services Utilization and Its Associated Factors in Tanzania: Evidence from Tanzania Demographic Health Survey 2015-16. Tanzania J Health Res. 2020;23:1-10.
- [CrossRef] [Google Scholar]
- Sustainable Development Goals and the Ongoing Process of Reducing Maternal Mortality. J Obstet Gynecol Neonatal Nurs. 2017;46:e56-64.
- [CrossRef] [PubMed] [Google Scholar]
- Maternal Mortality Measurement: Guidance to Improve National Reporting Geneva: World Health Organization; 2022.
- [Google Scholar]
- Strategies toward Ending Preventable Maternal Mortality (EPMM) Geneva: World Health Organization; 2015.
- [Google Scholar]
- WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience Geneva: World Health Organization; 2016.
- [Google Scholar]
- Health Facility Delivery in Sub-Saharan Africa: Successes, Challenges, and Implications for the 2030 Development Agenda. BMC Public Health. 2018;18:765.
- [CrossRef] [PubMed] [Google Scholar]
- WHO Recommendations on Postnatal Care of the Mother and Newborn Geneva: World Health Organization; 2014.
- [Google Scholar]
- Socioeconomic Inequalities in the Continuum of Care Across Women's Reproductive Life Cycle in Bangladesh. Sci Rep. 2022;12:15618.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of Inequality in Utilization of Maternal Healthcare Services between Bangladesh and Pakistan: Evidence from the Demographic Health Survey 2017-2018. Reprod Health. 2023;20:43.
- [CrossRef] [PubMed] [Google Scholar]
- Inequalities in the Utilization of Maternal Health Care in the Pre-and Post-National Health Mission Periods in India. J Biosoc Sci. 2020;52:198-212.
- [CrossRef] [PubMed] [Google Scholar]
- Inequalities in Maternal Health Care Utilization in Benin: A Population Based Cross-sectional Study. BMC Pregnancy Childbirth. 2018;18:194.
- [CrossRef] [PubMed] [Google Scholar]
- Socioeconomic Inequalities in Maternal Health Service Utilisation: A Case of Antenatal Care in Nigeria Using a Decomposition Approach. BMC Public Health. 2019;19:1493.
- [CrossRef] [PubMed] [Google Scholar]
- Socioeconomic and Geographic Variations in Antenatal Care Coverage in Angola: Further Analysis of the 2015 Demographic and Health Survey. BMC Public Health. 2020;20:1243.
- [CrossRef] [PubMed] [Google Scholar]
- Geographical and Socioeconomic Inequalities in the Utilization of Maternal Healthcare Services in Nigeria: 2003-2017. BMC Health Serv Res. 2020;20:849.
- [CrossRef] [PubMed] [Google Scholar]
- Socioeconomic Inequalities in Maternal Health Care Utilization and Delivery Channels in Nigeria. J Popul Soc Stud. 2023;31:672-95.
- [CrossRef] [Google Scholar]
- Prevalence and Socioeconomic Inequalities in Eight or More Antenatal Care Contacts in Ghana: Findings from 2019 Population-Based Data. Int J Womens Health. 2021;13:349-60.
- [CrossRef] [PubMed] [Google Scholar]
- Explaining Socioeconomic Disparities and Gaps in the Use of Antenatal Care Services in 36 Countries in sub-Saharan Africa. Health Policy Plan. 2021;36:651-61.
- [CrossRef] [PubMed] [Google Scholar]
- Poor Coverage and Quality for Poor Women: Inequalities in Quality Antenatal Care in Nine East African Countries. Health Policy Plan. 2021;36:662-72.
- [CrossRef] [PubMed] [Google Scholar]
- Socioeconomic Inequalities in Reproductive Health Care Services across Sub-Saharan Africa. A Systematic Review and Meta-Analysis. Sex Reprod Healthc. 2020;25:100536.
- [CrossRef] [PubMed] [Google Scholar]
- MoH. The Somaliland Health and Demographic Survey 2020. 2020 Available from: https://www.somalilandcsd.org/somaliland-health-anddemography-survey-slhd2020/
- [Google Scholar]
- Predictors of Maternal Health Services Uptake in West African Region: A Multilevel Multinomial Regression Analysis Of Demographic Health Survey Reports. Reprod Health. 2024;21:45.
- [CrossRef] [PubMed] [Google Scholar]
- Multilevel Analysis for Applied Research: It's just Regression! New York: Guilford Press; 2007.
- [Google Scholar]
- Inequities in the Uptake of Reproductive and Maternal Health Services in the Biggest Regional State of Ethiopia: Too Far From “Leaving No One Behind”. Clin Outcomes Res. 2020;12:595-607.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of the Capacity of Health Facilities in Preventing and Managing NonCommunicable Diseases in Selected Regions of Somaliland. Research Square [Preprint]; 2023
- [CrossRef] [Google Scholar]
- The Role of Geographical Access in the Utilization of Institutional Delivery Service in Rural Jimma Horro District, Southwest Ethiopia. Prim Heal Care Open Access. 2014;4:1.
- [Google Scholar]
- Inequalities in Maternal Health Care Utilization in Sub-Saharan African Countries: A Multiyear and Multi-Country Analysis. PLoS One. 2015;10:e0120922.
- [CrossRef] [PubMed] [Google Scholar]
- Socioeconomic Inequalities in the Uptake of Maternal Healthcare Services in Ethiopia. BMC Health Serv Res. 2017;17:367.
- [CrossRef] [PubMed] [Google Scholar]
- Inequities in Skilled Attendance at Birth in Namibia: A Decomposition Analysis. BMC Pregnancy Childbirth. 2011;11:34.
- [CrossRef] [PubMed] [Google Scholar]
- Inequities in Maternal Health Services Utilization in Ethiopia 2000-2016: Magnitude, Trends, and Determinants. Reprod Health. 2018;15:119.
- [CrossRef] [PubMed] [Google Scholar]






