Translate this page into:
2013~New Horizon With Rabies Biologicals
Abstract
Summary
Prevention is the only way out to stop death from Rabies, not the treatment of the same to cure the diseased. The only communicable ailment having 100% mortality depicts almost full preventive protection on the other side of the coin. The age old nerve tissue vaccine below the belly--dermis is ultimately history and almost half – a – dozen ultramodern Anti- rabies biological are on the cards now-a-days. Justified usage of them and social alertness reflecting the health consciousness of the civilization should improve the quality of human existence on the planet – let this be the theme of life in every sunrise to be seen. This Endeavour aims to reflect the light of management system of Anti-rabies prophylaxis with the most modern tools.
Introduction:
Hydrophobia is the end result of Rabies virus infection with variable incubation period from three weeks to three months in majority of victims. Treatment possibility being unable to achieve better prognosis, worldwide health agencies stress upon the preventive measures to be full proof at any cost. We the community health workers should make ourselves quite alert and dutiful to realize our responsibilities in this regard, to foresee a “Rabies-Free-India by 2020”.
Rabies has been classified as most dreaded fatal one, among all the infectious diseases, concerned to the civilization. It has the unique feature of mostly being accidental in origin with long incubation span and always considered to be the one way traffic, having no prognostic parameter.
Detected at the ancient age of Sushruta (later in the west) and Sanskrit (‘Rabies’ from ‘RAVAS’ – a synonym of violence), this threat of nature reigned unopposed till the Legendary Savior Louis Pasteur (and his colleague P.P. Emile Roux ) could vaccinate Joseph Mister with self-invented crude vaccine against Rabies virus on 6th. July,1885 and saved a life.
Epidemiology:
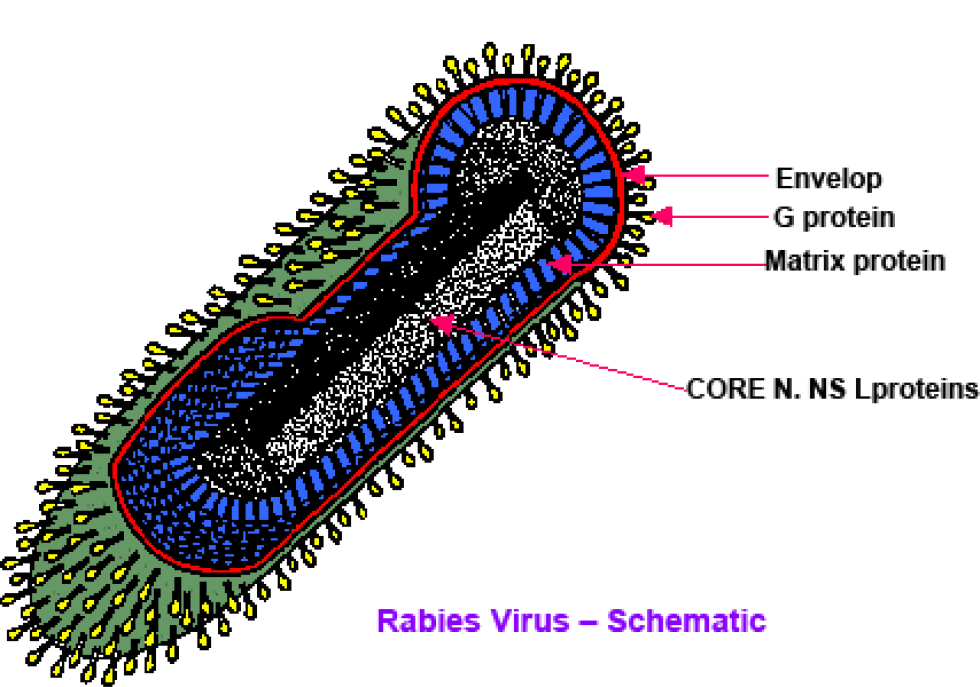
The causative factor, a fatal virulent RNA virus was identified and placed in Rhabdoviridae family as Lyssavirus genus -type I, covered by an envelope having spike-like projections (10 nm in length) corresponding to G-protein trimers which recognize specific viral receptors on susceptible cell membranes and accounting for virulence as well as antigenicity.1,2,3
Neurotropic in nature, this virus multiplies in neuro-muscular junctions and nerve tissues, invades the central nervous system via branches of neural network, aiming the cephalic terminal stations, wherefrom they follows the efferent distribution to affect the body organs and terminates human life unopposed.1
The invasion of virus in the humane is mostly accidental - through the involvement of an animal pre-infected by Rabies virus, and/or suffering from the disease itself. Bite, scratch or salivary contact of any infected/diseased animal, always proves fatal and needs instant attention and full prophylaxis at the earliest, considering the situation as a medical emergency. Local treatment of the wound including anti-tetanus measure followed by immunization (both Active & Passive) with vaccine and Rabies immunoglobulin is the complete package.4
All warm blooded mammals are susceptible to Rabies virus- as per W.H.O and text recommendations, but as far the spread of the disease is concerned, there exist some relaxations among the animal species on practical possibilities. In Indian sub-continent animals (pet, stray, domestic) usually involved are dogs, cats, mongoose, monkeys, pigs, horses and cattle as well. All wild animals are potentially risky in any sort of contact history. 1,2,5
Birds and rodents have not shown to have recognizable responsibilities as per human spread is concerned, on the records. As such avian, rat, mole, squirrel, lizard, scorpion, frog/toad, aquatic mammals and insects are usually acquitted of the charge. Indian bats are also classified out of the list, unlike those of western world.2,5
Among the 55,000 plus rabies victims more than 20,000 lives are lost every year in India, while 2.3 million persons receive post exposure treatment out of 17.5 million animal exposure victims yearly. All over India, this vector borne disease has been reported except Andaman, Nicobar and Lakshadweep islands which tallies with ‘sea barrier theory’..2,3,4
| Category | Type of contact with a suspect or confirmed rabid domestic or wild animal, or animal unavailable for observation | Recommended Treatment |
|---|---|---|
| I | Touching or feeding of animals. Licks on intact skin. | None, if reliable case history is available. |
| II | Nibbling of uncovered skin minor scratches or abrasions without bleeding. Licks on broken skin. | Administer vaccine immediately. Stop treatment if animal remainshealthy throughout an observation period of 10 days. |
| III | Single or multiple transdermal bites or scratches. Contamination of mucous membrane with saliva (i.e. licks). | Administer rabies immunoglobulin and vaccine immediately. Stop treatment if animal remains healthy throughout an observation period of 10 days. |
Post & Pre Exposure Prophylaxis
Modern medicine emphasizes on full and total prophylactic attitude only, as a clear and final measure. This process is bound to follow the rule of three, which states as described by three words :
Urgent
Immediate
Instant.
Confusions, hesitations, delay and relaxation of the prophylactic vaccination rules, attracts the only and inevitable judgment of nature - catastrophe - in other words “Termination of human life ”
The prophylactic post exposure immunization comprises two parts :
Active Immunization : By tissue culture anti-rabies vaccine by either intramuscular or intradermal schedule.
Passive Immunization : By Rabies Immunoglobulin either of equine or of human origin.
Schedules of vaccination (Active Immunization) :1,2,4,5 Intramuscular Essen schedule
Post Exposure Prophylaxis (i.m):
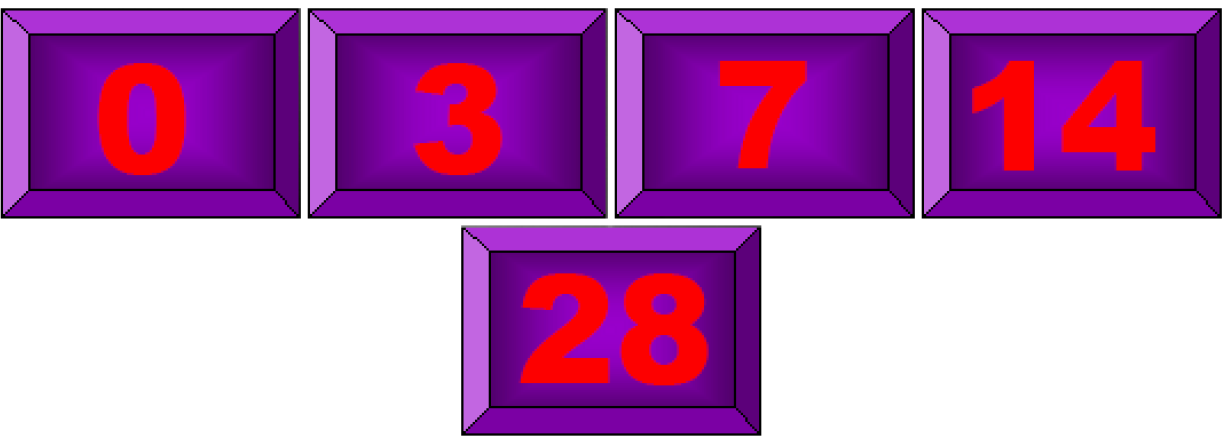
One vial deep i.m in alternate deltoid on days
Intradermal Updated Thai Red Cross Schedule.
Post Exposure Prophylaxis (i.d)
0. 1 ml of i.m dose in both deltoid skin layers on days
An important thing to remember : ‘0’ day always indicates the 1st dose day in both the schedules.
Proper technique for intradermal vaccination should be adopted - any sort of compromise must be regretted.
Dose miss on scheduled date can be allowed a relaxation of one single day only, beyond which a rescheduled vaccination in mandatory.
Pre - exposure vaccination schedule (presumptive vaccination) is designed as :
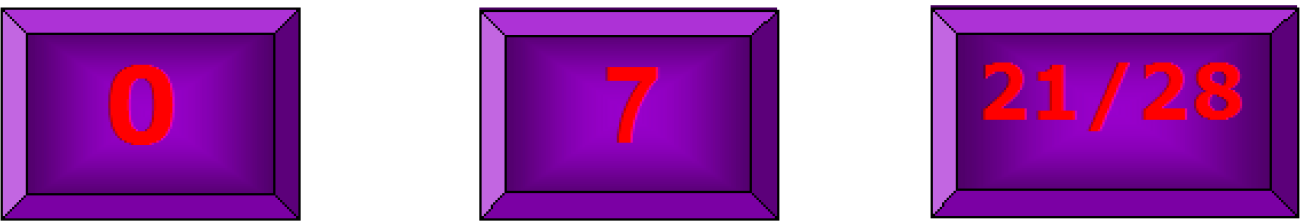
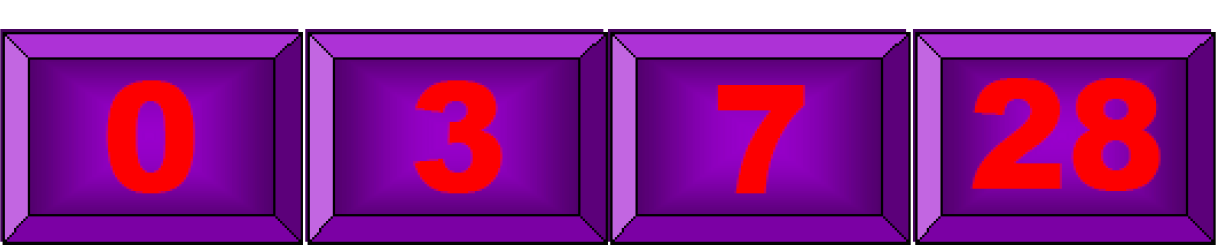
{ Intramuscular dose : One vial deep i.m in alternate deltoid. Intradermal dose : 0.1 ml of i.m dose in single deltoid skin layers.}
Booster : On completion of 1st. year then every 5 yearly if rabies virus neutralizing antibody titre (quantitative) falls to < 0.5 IU/ml.4
Re - exposure vaccination schedule (Re-vaccination) is designed as : (For previously vaccinated people either by Pre or Post Exp. schedule)
{ Intramuscular dose : One vial deep i.m in alternate deltoid. Intradermal dose : 0.1 ml of i.m dose in single deltoid skin layers. }
Passive Immunization (With Rabies Immunoglobulin either of equine or of human origin):
[In all Category III exposure victims]
A. Equine Rabies Immunoglobulin : 40 I.U. per kg body weight into and around the wound.
B. Human Rabies Immunoglobulin : 20 I.U. per kg body weight into and around the wound.
Passive Immunization (With Rabies Immunoglobulin either of equine or of human origin) should take place within the 7th day of the 1st dose of vaccine in all schedules.1
Rabies Immunoglobulin must be used, if the initiation of the treatment is delayed even, in all Category III exposure victims.1,2
Passive Immunization (With Rabies Immunoglobulin) is not indicated in all Category III exposure victims having confirmed & documented history of either Pre or Post exposure vaccination.4
Wound toileting with detergent soap under running water, OVER 10 MINUTES is a must, to reduce the viral load at the area of exposure, and, is mandatory - as per W.H.O PROTOCOL.
The Government health service provides a comprehensive, responsible, latest & modern rabies prophylaxis system upto the grass root level as far as practicable, alongwith extensive trainings in multi-tire approach, initiating at officers’ training at Institute of Health & Family welfare to the district level covering the entire state of West Bengal.
The current treatment system is almost full-proof if exercised as per norms and proper procedures, with potent & safe Rabies Biologicals as per protocol, without any delay and with a little justified expertise.3
REFERENCES:
- Technical Report Series 931 (WHO EXPERT CONSULTATION ON RABIES- Geneva) - World Health Organization. 2005
- [Google Scholar]
- Laboratory Diagnostic Techniques-2007- ZOONOSIS DIVISION -- National Institute of Communicable Diseases (WHO Collaborating Centre for Rabies Epidemiology) - Delhi.
- [Google Scholar]
- The changing scenario of rabies in India: Are we moving towards its prevention and control? The Indian J Public Health. 2007;51(3):145-147.
- [Google Scholar]
- Park's text book of preventive and social medicine. (22nd). Jabalpur, India: M/s Banarasidas Bhanot publishers; 2013.
- [Google Scholar]





